The question of preoperative anxiety and depression in older patients and family protectors
Article information
Abstract
Background
Higher levels of anxiety increase the risks of surgery, including morbidity and mortality. The objectives of this study were to measure anxiety and depression during the preoperative period and to identify the degree of knowledge and concerns of older patients and their family protectors regarding anesthesia, and the causes of these concerns.
Methods
We administered a questionnaire to older patients scheduled to undergo surgery and their family protectors one day prior to the surgery. The questionnaire included tools for quantifying anxiety and depression (Anxiety-Visual Analogue Scale, the Amsterdam Preoperative Anxiety and Information Scale, State-Trait Anxiety Inventory Korean YZ Form, and Short Form Geriatric Depression Scale). We also asked about the concrete causes of anxiety using pre-created forms.
Results
There were 140 older patients and family protectors who participated in the study. The majority of older patients (n = 114, 81.4%) undergoing surgery and their family protectors (n = 114, 81.4%) indicated that they were anxious. Most of the older patients and their family protectors responded that they had insufficient knowledge about anesthesia, and they were mostly worried about failure to awaken following surgery, and postoperative pain. Older patients with higher anxiety scores showed higher depression scores. There were significant differences in depression scores depending on the presence of cohabitating family members.
Conclusions
It is important to remember that older patients with higher depression scores have higher anxiety during the preoperative period.
INTRODUCTION
Anxiety for patients undergoing surgery is a common emotional response. Many individuals have misperceptions or vague anxiety about anesthesia, whether they have received information from a surgeon or have obtained fragmentary information about anesthesia via the Internet or from other individuals. Excessive anxiety can affect immune mechanisms through the release of corticosteroids and may be associated with abnormal hemodynamics as a consequence of endocrine changes or autonomic variation. Higher levels of anxiety increase the risks of surgery, including morbidity and mortality [1,2]. Specifically, stress can lead to delayed wound healing, increased risk of postoperative complications, greater demand for painkillers, and extension of hospital stay, along with increased risk of mortality and morbidity [2]. Therefore, it is important to reduce preoperative anxiety for good prognosis and patient comfort [3].
Degeneration of the autonomic nervous system occurs gradually with aging, leading to gradual reduction in an individual’s ability to adapt [4]. In addition, the homeostatic balance is more easily altered by exogenous stimuli [5]. Older patients facing surgery may be more vulnerable to this physiological response [6]. Anxiety may be caused by anesthesia, surgery, and recovery, among others [7]. Depression is also a common problem in older patients, causing emotional suffering and increased mortality [8]. Therefore, for an older patient undergoing surgery, anxiety and depression are issues that must be addressed together [9]. Early interventions to minimize preoperative anxiety and the stress response may affect outcomes [1,8,10]. The purposes of the present study were to measure anxiety and depression during the preoperative period, and to identify the degree of knowledge and concerns of older patients and their family protectors with respect to anesthesia, as well as the causes of these concerns. Ultimately, we provide relief by providing information to patients and their family protectors.
MATERIALS AND METHODS
Study design
This cross-sectional study was reviewed and approved by the institutional review board (no. 19-0033), and written informed consent was obtained prior to the interviews.
Study subjects consisted of one set of older patients and family protectors. The patients included were 65 years of age or older; inpatients undergoing elective surgery under general or regional anesthesia; and individuals who could understand the study questionnaire. The exclusion criteria were as follows: (1) individuals with difficulty completing the survey and interviews; and (2) patients taking prescribed sedatives and antidepressants or anxiolytics. Family protectors included in the study were in the same room as the patient when the questionnaire was administered. Relationships between older patients and their family protectors included spouse, child, daughter-in-law, son-in-law, or sibling. When there were two or more possible family protectors, we selected the first applicants among these individuals.
To calculate the number of samples we used G*Power 3.1.9.2 with the alpha error set at 5% and power set at 95%, effect size at 15%, number of predictors at 4 (number of key metrics in questionnaire questions: (Anxiety-Visual Analogue Scale [A-VAS], Amsterdam Preoperative Anxiety and Information Scale [APAIS], State-Trait Anxiety Inventory Korean YZ Form [STAI-KYZ], Short Form Geriatric Depression Scale [SGDS]), F-test, and linear multiple regression. Based on these calculations, a sample size of 129 individuals was required in the study, and a total of 140 people were selected, allowing for dropouts. Effect size and power referred to the values suggested by Cohen.
Surveys and interviews were conducted in the ward on the day before surgery. After a brief explanation by the researcher, older patients and their family protectors were asked to complete the questionnaire. During the survey, when an individual asked the researcher a question about an item on the questionnaire, the explanation was repeated. Factors known to influence anxiety such as calmness, open attitude, and friendly atmosphere were kept the same for all older patients and their family protectors. It took about 15 min for the individuals to complete the questions. Data regarding sociodemographic factors (age, sex, religion, educational background, economic power, marital status, family number, cohabitation status) and medical history were obtained directly inquired from patients and their family protectors.
We used self-reported structured questionnaires (A-VAS, APAIS, STAI-KYZ, SGDS) and questionnaire developed for this study.
The contents of the questionnaires for older patients and family protectors were different. The questionnaires for the older patients were composed of a total of 8 questions, and those for their family protectors consisted of a total of 6 questions. The questionnaire used in the study is shown in Supplementary Material. Commonly used tools for older patients and their family protectors are the A-VAS and the APAIS. As additional tools for the older patients only, we selected the anxiety state version of the STAI-KYZ and the SGDS. We also asked the individuals about their specific knowledge of anesthesia (Cronbach’s α [reliability coefficient] was 0.7 and 0.6 for older patients and their family protectors, respectively) and the concrete causes of anxiety regarding anesthesia and surgery (Cronbach’s α 0.7 and 0.6 for older patients and their family protectors, respectively) using the survey questions we designed.
Anxiety measuring tools
The A-VAS is a scale graded with a score from 1 (slightly anxious) to 10 (extremely anxious). Values of A-VAS around 5 are a reliable threshold for a clinically meaningful level of preoperative anxiety [11].
The APAIS consists of 6 questions using a five-point Likert scale (1: never, 2: low, 3: moderate, 4: strong, 5: extreme) and assesses anxiety state (1st, 2nd, 4th, 5th questions of the APAIS) and desire for information related to surgery and anesthesia (3rd, 6th questions of the APAIS). An APAIS anxiety subscore of 11 points or more indicates a significant anxiety state. A score with respect to desire for information of 8 points or more means that an individual would like to know as much as possible about anesthesia or surgery [12,13]. Cronbach’s α of the APAIS used in this study was 0.9 for older patients and 0.9 for their family protectors. In the APAIS, Cronbach’s α of the 4 questions (1st, 2nd, 4th, 5th questions of the APAIS) representing anxiety with respect to anesthesia and surgery was 0.8 for older patients and 0.8 for their family protectors. Cronbach’s α of the 2 questions (3rd, 6th questions of the APAIS) representing the need for information was 0.8 for older patients and 0.8 for their family protectors.
The STAI-KYZ contains 20 questions each for anxiety state and trait, respectively (with 40 questions in total). Anxiety state represents a situational emotional state by subjective feelings of fear and tension. We only used the 20 questions rated on a 4-point scale (1: not at all, 2: somewhat, 3: moderately, 4: very much so) for anxiety state in the STAI-KYZ in this study. Out of the 20, 10 questions (3rd, 4th, 6th, 7th, 9th, 12th, 13th, 14th, 17th, 18th questions of the STAI-KYZ) are worded in a way such that higher scores indicate greater anxiety (e.g., ‘tense’). On the other hand, the remaining 10 questions (1st, 2nd, 5th, 8th, 10th, 11th, 15th, 16th, 19th, 20th questions of the STAI-KYZ) are negatively loaded and must be reverse-scored to reduce the effects of acquiescence (e.g., ‘am happy’). A cutoff point of 54–55 on the STAI-KYZ has been suggested to detect clinically significant symptoms of anxiety for older adults [14]. Cronbach’s α of the STAI-KYZ was 0.7 in the present study.
Depression measuring tool
The SGDS contains 15 questions that are answered "yes" or "no". In scoring the SGDS, each item is scored 0 or 1 depending upon whether the item is worded positively (‘am depressive’) or negatively (‘am happy’). That is, the 1st, 5th, 7th, 11th, 13th questions of the SGDS are negatively loaded (‘am happy’) and must be reverse-scored. Scores on the SGDS range from 0 to 15, and a score > 5 points is suggestive of depression, with a score ≥ 10 points almost always indicative of depression [8,15]. Cronbach’s α of the SGDS was 0.6 in this study.
Statistical analysis
Statistical analysis was performed using MedCalc Software Version 17.1 for Windows (Medcalc Software, Belgium) and Graphpad Prism Software Version 8 (Graphpad Software Inc., USA). A P value < 0.05 was considered statistically significant.
Assessment of the relationship between environmental factors and anxiety or depression was performed using correlation analysis (Pearson correlation coefficient or Spearman’s coefficient of rank correlation) and one-way analysis of variance (ANOVA). We used medium 0.15 of effect size f2 commonly used in regression analysis and correlation analysis.
RESULTS
None of the older patients or family protectors withdrew from the present study. Finally, 140 older patients and 140 family protectors participated in our study.
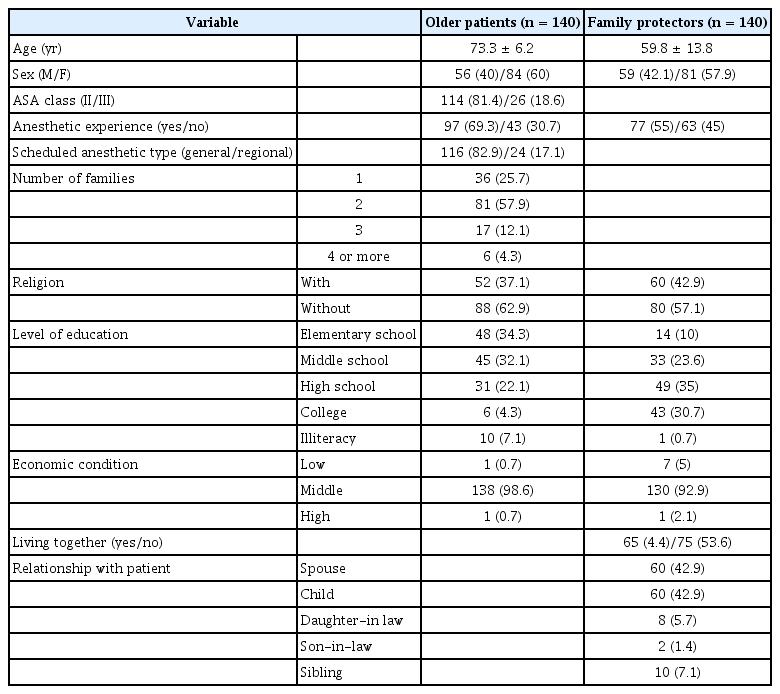
Characteristics of the older patients and their family protectors are presented in Table 1.
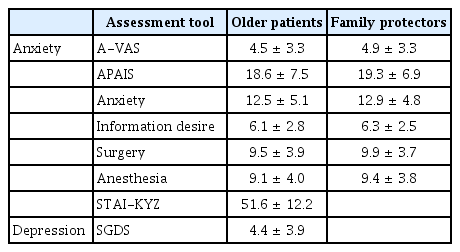
Older patients (n = 114, 81.4%) and their family protectors (n = 114, 81.4 %) answered yes to the question, ‘‘are you anxious ahead of surgery?’’. Among them, 103 older patients and family protectors replied equally. Fig. 1 shows the A-VAS distribution of the patients (Fig. 1A) and their family protectors (Fig. 1B). The reliability threshold of the A-VAS is 5 points, and the mean value of the A-VAS in older patients was 4.5 ± 3.3 compared to 4.9 ± 3.3 in their family protectors (paired t-test, P = 0.115). There was a statistically significant moderate positive linear correlation (r = 0.383, P < 0.001) between the A-VAS of the older patients and their family protectors.
Distribution of A-VAS in older patients (A) and family protectors (B). A-VAS: anxiety visual analogue scale.
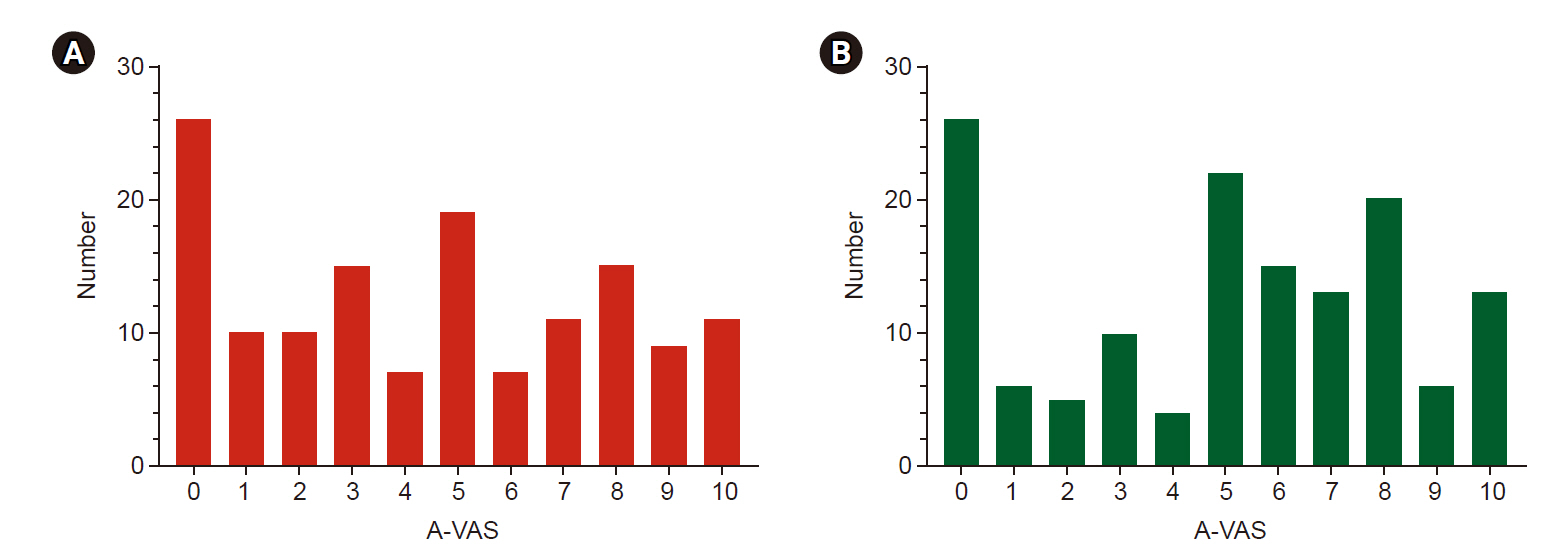
The mean values of the anxiety score (A-VAS, anxiety subscores of APAIS and STAI-KYZ) of older patients and their family protectors and the depression score (SGDS) of older patients are shown in Table 2. There was a possitive correlation between the A-VAS, the anxiety subscore of the APAIS, and the STAI-KYZ, an an instrument for assessing anxiety. The specific results of the correlation analysis of anxiety assessment tools were as follows: between A-VAS and anxiety subscore of APAIS (r = 0.684, P < 0.001); between A-VAS and STAI-KYZ (r = 0.681, P < 0.001); between anxiety subscore of APAIS and STAI-KYZ (r = 0.659, P < 0.001) in older patients, and between A-VAS and anxiety subscore of APAIS (r = 0.644, P < 0.001) in family protectors. The mean APAIS anxiety subscores were 12.5 ± 5.1 and 12.9 ± 4.7, respectively, in older patients and their family protectors. In this study, the mean values of the STAI-KYZ were 54.2 ± 11.3 and 40.1 ± 9.4 for the patients who answered that they were anxious and not anxious, respectively, and there was a significant difference (P < 0.001). More than half of the patients (n = 80, 57.1%) and their family protectors (n = 72, 51.4%) answered that they had insufficient knowledge about the anesthesia administered during surgery (Fig. 2). The degree of knowledge regarding anesthesia was not correlated with previous anesthesia history (rho = 0.074, P = 0.386) and had no influence on anxiety scores (rho = –0.102, P = 0.232 for A-VAS, rho = –0.065, P = 0.444 for anxiety subscore of APAIS ) in older patients. After the interviews, it was found that a significant number of older patients and their family protectors were anxious about the possibility of failure to awaken following surgery, and postoperative pain, in order (Table 3).
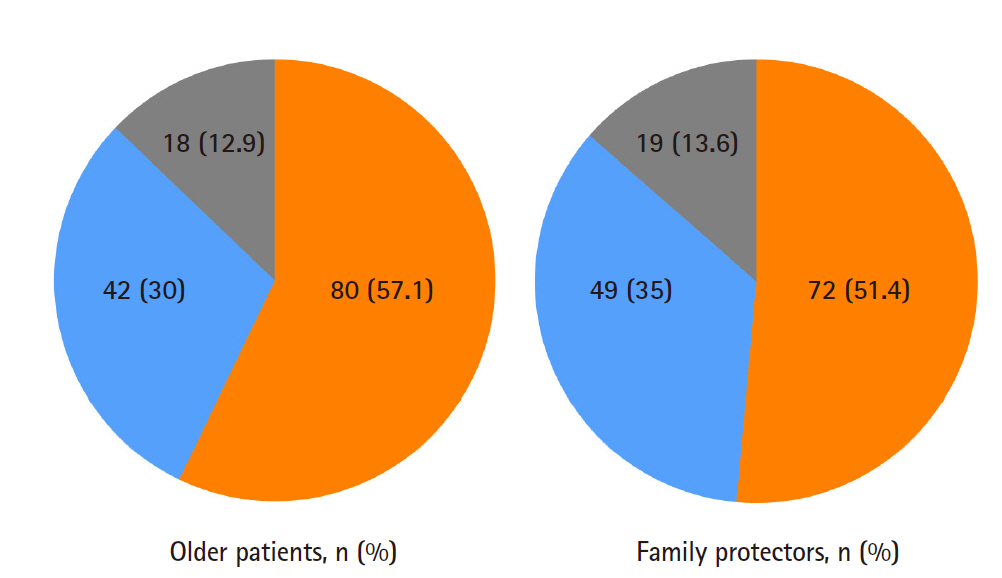
Degree of knowledge about anesthesia of older patient and family protectors. The answer to the 4th question in the questionnaire, “How much do you know about anesthesia done during surgery?”, orange: the number (%) of persons answered “I have no idea.”, blue: the number (%) of persons answered “I know a little.”, gray: the number (%) of persons answered “I know it well.”
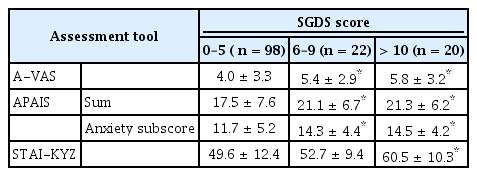
According to the SGDS scores, there were three groups: 0–5 points (normal), 6–9 points (suggestive of depression), 10–15 points (indicative of depression), and the number of patients in each group was 98 (70%), 22 (15.7%), and 20 (14.2%), respectively. Table 4 shows the anxiety scores (A-VAS, anxiety subscore of APAIS, STAI-KYZ) by group divided by SGDS score. The higher the anxiety score (A-VAS, anxiety subscore of APAIS, STAI-KYZ), the higher the depression score (SGDS) (Fig. 3).

Association between the SGDS score and the A-VAS (A), anxiety subscore of APAIS (B) or STAI-KYZ (C). (A) The red solid line represents linear regression of SGDS vs. A-VAS (A-VAS = 0.2469 × SGDS + 3.392, P < 0.001) and red dotted lines represent 95% confidence interval (CI). Green filled circles show distribution of A-VAS score. (B) The red solid line represents linear regression of SGDS vs. Anxiety subscore of APAIS (Anxiety subscore of APAIS = 0.3743 × SGDS + 10.88, P = 0.001) and red dotted lines represent 95% CI. Blue filled circles show distribution of Anxiety subscore of APAIS score. (C) The red solid line represents linear regression of SGDS vs. STAI-KYZ (STAI-KYZ = 1.178 × SGDS + 46.40, P < 0.001) and red dotted lines represent 95% CI. Grey filled circles show distribution of STAI-KYZ. SGDS: Short Form Geriatric Depression Scale, A-VAS: anxiety visual analogue scale, Anxiety subscore of APAIS: Anxiety subscore of Amsterdam preoperative anxiety information scale, STAI-KYZ: State Trait Anxiety Inventory Korean YZ Form.
The A-VAS, anxiety subscore of APAIS, and STAI-KYZ scores were higher in older female patients than in older male patients. No statistically significant differences were detected in either anxiety and depression scores in older patients and family protectors’ according to previous experience with anesthesia, scheduled anesthetic type (general anesthesia or regional anesthesia), or American Society of Anesthesiologists physical status class. We classified the operations as “minor” or “major” to evaluate the differences in anxiety and depression scores according to the type of surgery. ‘‘Minor’’ was defined as less invasive surgery of limited duration (< 2 h) (non-cancer surgery, minor orthopedic surgery, diagnostic procedure, arthroscopies, laparoscopies, inguinal hernia). Operations classified as ‘‘major’’ were extensive operations with a high impact and long duration (≥ 2 h) (cancer surgery, laryngectomy, cardiac surgery, brain surgery, spine or hip surgery). There were no significant differences in the A-VAS, APAIS, STAI-KYZ, and SGDS scores of older patients according to major or minor surgery. In contrast, the A-VAS of family protectors showed a significant difference (P = 0.03).
Anxiety scores (A-VAS, anxiety subscore of APAIS, STAI-KYZ) did not significantly differ depending on the presence of cohabitating family members, while there were significant differences in the depression score (SGDS) (P = 0.019). That is, the SGDS mean score of patients living alone was 5.8 ± 4.6, while that of patients living with a family was 3.9 ± 3.6.
A significant difference in the desire for information in older patients was detected on the APAIS according to degree of education (P = 0.023). That is, older patients who graduated from college (9.2 ± 0.9) had a stronger desire to know about anesthesia or surgery than those who graduated from elementary school (5.6 ± 2.7). However, there were no differences in the anxiety subscores of the APAIS according to the level of education, or in the A-VAS, STAI-KYZ, or SGDS. The religiosity and economic situation of the patients also did not affect the anxiety scores or depression scores.
DISCUSSION
The aim of the current study was to investigate the degree of preoperative anxiety and depression and the specific reasons for these concerns in older patients undergoing surgery and their family protectors. The point that differentiates our study from others was that the older patients and their family protectors were both subjected to our investigation [1,16,17]. High levels of preoperative anxiety are known to cause many changes in physical function. Older patients, with decreased reserves as a result of the aging process, are more vulnerable to these changes than are healthy young patients.
Our findings indicated the presence of a statistically significant correlation (r = 0.383, P < 0.001) in the A-VAS scores between older patients and their family protectors. Most of the family protectors of older patients present during the interview were spouses or children. Based on the information described above, our authors assumed that the degree of anxiety of family protectors might be higher than that of older patients. There is research supporting the idea that family members feel anxiety during the preoperative period and that their STAI anxiety-state scores are higher than those of the surgical patients [18]. However, unlike our predictions, we did not find significant differences in the anxiety scores of older patients and their family protectors in the present study.
Most of the older patients and their family protectors surveyed responded that they had not received enough knowledge about anesthesia prior to surgery. In older patients, no difference was seen in the anxiety scores for surgery and anesthesia in the APAIS, but family protectors were significantly more worried about surgery than anesthesia. Interestingly, older patients (n = 26, 18.6%) and their family protectors (n = 26, 18.6%) responded that they were not anxious even before surgery. This finding might indicate that the individuals’ fear of surgery was really low, or that they placed a great deal of faith in the medical staff.
Depression scores (SGDS) showed a significant positive linear correlation with anxiety scores in older patients. Older patients with depression scores between 0 and 5 had different anxiety scores compared to those with depression scores 6 or higher. In other words, older patients with a depression score of 6 or higher had a higher anxiety score compared to those with a depression score less than 5. Depression and anxiety are two common mental health concerns among older patients [19]. These results suggest that it is important to pay greater attention to interventions in both anxiety and depression in older patients during the preoperative period.
The present study revealed that older female patients have higher anxiety scores than older male patients. There are many studies in the literature that corroborate the results of our study [20,21]. The authors of the current study believe that the low anxiety scores in the male patients were the results of a tendency to not easily reveal their feelings. An earlier study reported that previous experience of surgery decreases the degree of anxiety [22]. However, we found that previous anesthetic experience and anxiety levels were not correlated, although many of the participants (n = 97, 69.3%) had experienced anesthesia before.
Another study suggested that patients with more education are more anxious [23]. The more educated individuals were more likely to be active in their expression of anxiety. However, in the present study, no correlation of education with anxiety score was observed in older patients and their family protectors. In older patients who graduated from college, the desire to know about anesthesia was greater than that in patients who graduated from elementary school. We anticipated that the older patients without religion would be more nervous during the preoperative period than those who had religion. Indeed, there was a previous study to support this presumption [23]. Contrary to expectations, however, religion was not associated with any difference in anxiety scores in the present study.
McCleane and Cooper [24] reported that the most frequent survey responses in research investigating the reasons for preoperative anxiety were postoperative pain, awakening during surgery, waiting time before surgery, nausea and vomiting, and loss of inhibition due to anesthesia. Our study showed the reasons for anxiety before surgery were mainly postoperative pain and fear regarding failure to awaken following anesthesia. Unlike other studies, the degree of fear of waking up during surgery was low [7].
A limitation of this study arises from the fact that the degree of anxiety may vary according to the place and time of the administration of questionnaires. We interviewed patients admitted the day before surgery, but difference in the degree of anxiety between the day before surgery and the day of surgery will surely exist.
In conclusion, older patients undergoing surgery were not only anxious but also depressive, factors which should not be overlooked. When visiting older patients preoperatively, anesthesiologists should deal with concerns regarding postoperative pain and the fear of failing to awaken following anesthesia. In the present study, the older patients showed similar anxiety regarding anesthesia or surgery, but the family protectors showed higher anxiety for surgery than for anesthesia. Therefore, not only explanations or efforts on the part of the anesthesiologist, but also on the part of the surgeon are necessary. Providers should attempt to reduce the vague anxiety caused by lack of knowledge regarding anesthesia through sufficient communication with older patients and their family protectors to build trust with these individuals.
SUPPLEMENTARY MATERIALS
Supplementary data (survey questionnaire for older patients) are available at https://doi.org/10.17085/apm.2020.15.2.217
Notes
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
AUTHOR CONTRIBUTIONS
Conceptualization: Seunghee Ki. Data acquisition: Younmi Oh, Sungho Moon, Kwangrae Cho, Myoung-hun Kim. Formal analysis: Seunghee Ki. Supervision: Sehun Lim. Writing—original draft: Younmi Oh. Writing—review & editing: Sehun Lim, Seunghee Ki.