Preoperative cephalhematoma size measured with computed tomography predicts intraoperative bleeding in pediatric patients undergoing cranioplasty
Article information
Abstract
Background
Cranioplasty for the treatment of cephalhematomas in small infants with limited blood volume is challenging because of massive bleeding. This study aimed to elucidate the correlation between cephalhematoma size and intraoperative blood loss and identify criteria that can predict large intraoperative blood loss.
Methods
We reviewed the medical records of 120 pediatric patients aged less than 24 months who underwent cranioplasty for treatment of a cephalhematoma. The cephalhematoma sizes in preoperative brain computed tomography (CT) were measured using ImageJ.
Results
Pearson correlation showed that the cephalhematoma size in the pre-operative brain CT was weakly correlated with intraoperative blood loss (Pearson coefficient = 0.192, P = 0.037). In a multivariable logistic regression analysis, a cephalhematoma size greater than 113.5 cm3 was found to be a risk factor for large blood loss. The area under the curve in the receiver operating characteristic plot of the multivariable model was 0.714 (0.619–0.809).
Conclusions
A cephalhematoma size cutoff value of 113.5 cm3, as measured in the preoperative CT imaging, can predict intraoperative blood loss exceeding 30% of the total body blood volume. The establishment of a transfusion strategy prior to surgery based on cephalhematoma size could be useful in pediatric cranioplasty.
INTRODUCTION
A cephalhematoma, which is a collection of blood between the skull and the periosteum, usually occurs in the neonatal period as a result of birth trauma. In most cases, the cephalhematoma is self-absorbed within 4 weeks; however, if it is not absorbed within this period, delayed ossification or calcification occurs [1]. The treatment of ossified cephalhematomas is controversial, and conservative treatment is recommended because of the possibility of natural absorption within 3–6 months. However, surgical treatment is required to prevent the development of asymmetry and skull deformities due to large cephalhematomas [2]. Cosmetic reasons are another indication for surgical treatment [3]. Performing surgery in patients at an early age, approximately 2 months old, is technically easy, and it provides the advantage of obtaining good head shape due to natural molding [4].
However, small infants with limited total blood volume might become hemodynamically unstable even with a relatively small amount of intraoperative bleeding. Along with the monitoring of vital signs and hemoglobin levels, visual estimation of blood loss in the surgical field is essential, but it is often inaccurate and unreliable [5]. Anesthesiologists should consider the possibility of massive bleeding and establish a fluid and transfusion strategy prior to the start of surgery. Total body blood volume should be an important consideration when deciding to perform transfusion in pediatric patients undergoing craniofacial surgery [6]. Thus, the prediction of intraoperative large blood loss based on the total body blood volume prior to surgery could be advantageous in establishing intraoperative transfusion strategies.
In this study, we measured the size of cephalhematomas in preoperative computed tomography (CT) images to elucidate the correlation between the cephalhematoma size and intraoperative blood loss. Additionally, we attempted to identify a cephalhematoma size cutoff value that can predict intraoperative blood loss exceeding 30% of the total body blood volume.
MATERIALS AND METHODS
Study population and data collection
The study protocol was approved by the Institutional Review Board of the University Health System, Seoul, South Korea (no. 4-2018-0701). Since the study involved retrospective review of patient medical records, the need for informed consent was waived. The medical records of pediatric patients aged less than 24 months who underwent cranioplasty for a cephalhematoma between January 2008 and March 2018 were retrospectively reviewed. During this period, the surgical procedure was performed by two surgeons. Linear skin incision is made on the longest dimension of the ossified mass. The pericranium is preserved for postoperative bony healing. Abnormal bony mass is removed using rongeur and high-speed drill to smoothen the edge of the bony mass. Bone bleeding is controlled using bone wax. Drainage catheter is inserted, and skin closure is done using absorbable monofilament suture in a subcuticular fashion. The exclusion criteria were as follows: age > 24 months, a previously diagnosed bleeding disorder, and insufficient medical data.
The following preoperative data were assessed: demographic data, laboratory data (hemoglobin, hematocrit, and platelet levels; prothrombin time; and international normalized ratio), and any preexisting conditions, including a history of congenital heart disease or neonatal jaundice. The assessed intraoperative data included duration of surgery, duration of anesthesia, intraoperative fluid amount, amount of packed red blood cells transfused, blood loss, urine output, intraoperative hypotension, severe hypotension, and vasopressor use. The following postoperative data were assessed: laboratory data (hemoglobin and hematocrit levels), postoperative transfusion of packed red blood cell or freshly frozen plasma, and duration of the postoperative hospital stay. Hypotension was defined as a 20% reduction in systolic blood pressure from baseline [7]; more than 50% reduction in systolic blood pressure from baseline was considered severe hypotension.
Patients were divided into two groups: large blood loss group and small blood loss group. Patients whose intraoperative bleeding exceeded 30% of the total body blood volume were classified as the large blood loss group. All others were classified into the small blood loss group. The estimated blood volume (ml) was calculated by multiplying the body weight (kg) by 80 ml.
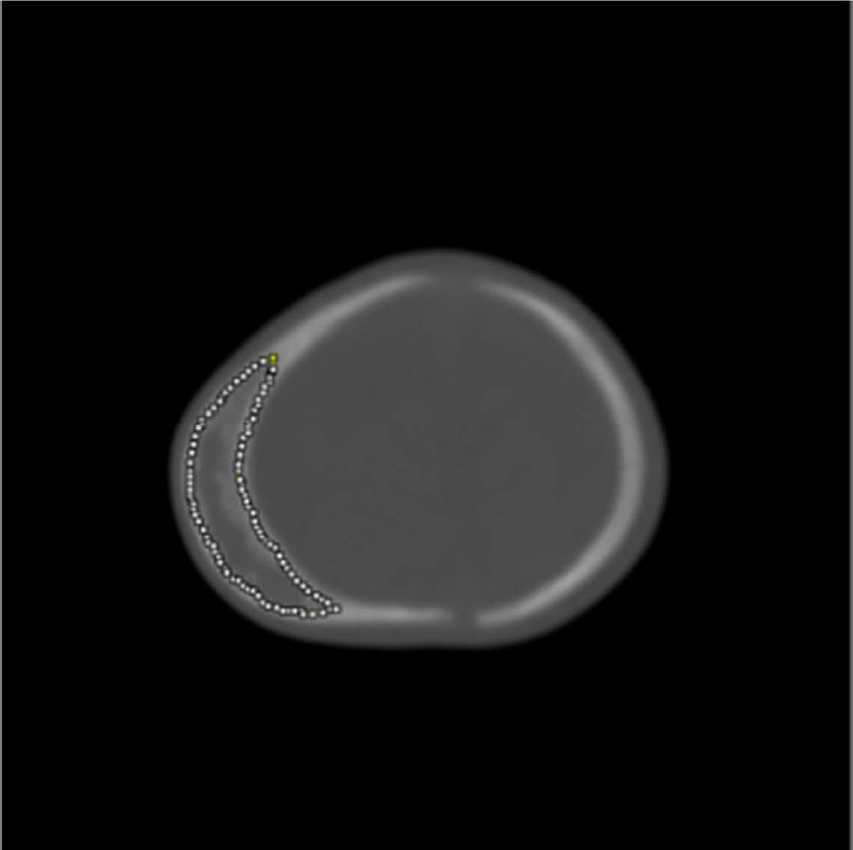
Each patient in this study underwent a preoperative brain CT for a cephalhematoma, and the size of the cephalhematoma was measured using ImageJ (version 1.33, U.S. National Institutes of Health, USA). Brain CT images were opened in ImageJ and the cephalhematomas were manually outlined on each slice (Fig. 1). The area of each hematoma was multiplied by the slice thickness to calculate the total volume.
Statistical analysis
Descriptive data are presented as mean values ± SD, or median (1Q, 3Q). For intergroup comparisons, the chi-square test or Fisher’s exact test was used for categorical variables and Student’s t-test or the Wilcoxon-Mann-Whitney test was used for continuous variables. Pearson correlation was used to determine the relationship between the two continuous variables. The binary response of the blood loss groups was analyzed by multivariable logistic regression in terms of explanatory variables: cephalhematoma size, age (months), weight, and American Society of Anesthesiologists’ physical status. We determined the cutoff value of the cephalhematoma size that maximized the area under the curve (AUC) when divided into two categories. Statistical analyses were performed using SPSS Statistics 23 (IBM SPSS Statistics for Windows, IBM Corp., USA), SAS (version 9.4, SAS Inc., USA), and R version 3.5.1 (The R Foundation for Statistical Computing, Austria).
RESULTS
A total of 123 pediatric patients underwent cranioplasty as treatment of a cephalhematoma from January 2008 to March 2018. Two patients aged > 24 months and one patient with incomplete data were excluded, and the remaining 120 patients were analyzed in this study. Of the final 120 patients analyzed, 32 were classified into the large blood loss group and 88 patients were classified into the small blood loss group.
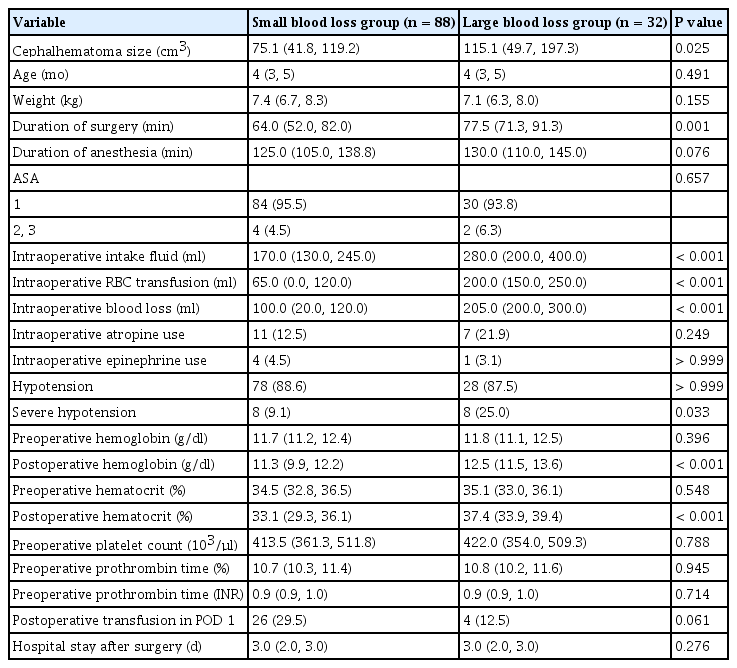
Demographics
Demographic data including age, body weight, and American Society of Anesthesiologists physical status were similar between the two groups; however the cephalhematoma size was higher in the large blood loss group than in the small blood loss group. While the incidence of intraoperative hypotension and atropine use were comparable between the two groups, the duration of surgery, amount of intraoperative packed red blood cells transfused, and the occurrence of severe hypotension were higher in the large blood loss group than in the small blood loss group. While the hemoglobin and hematocrit levels decreased during surgery in the small blood loss group (both P = 0.002), the change in the hemoglobin and hematocrit levels in the large blood loss group was not statistically different (P = 0.067 and P = 0.081, respectively). Postoperative transfusion and the length of hospital stay after surgery were comparable between the two groups (Table 1).
Relationship between cephalhematoma size and blood loss
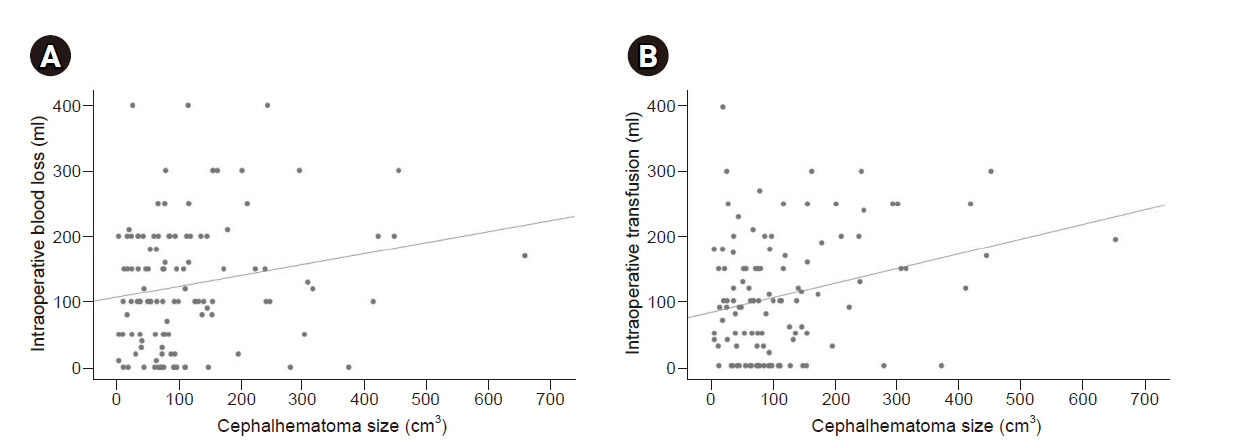
Pearson correlation showed that the cephalhematoma size measured in the preoperative brain CT scan was correlated with intraoperative blood loss (P = 0.037); however, the correlation between the two variables was weak (Pearson coefficient = 0.192; Fig. 2A). Cephalhematoma size was also weakly correlated with the amount of packed red blood cells transfused (Pearson coefficient = 0.273, P = 0.003; Fig. 2B).
Cephalhematoma size as a risk factor for large blood loss
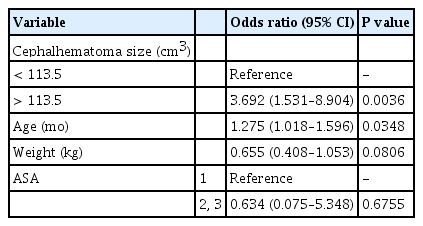
In the multivariable regression analysis, only age was found to be a risk factor for large blood loss (Table 2). The cephalhematoma size was transformed into a binary variable using a cutoff value of 113.5 cm3 obtained by maximizing the AUC (Fig. 3A). In a multivariable logistic regression analysis with categorized cephalhematoma size as the variable, a cephalhematoma size greater than 113.5 cm3 was found to be a risk factor for large blood loss (Table 3). The AUC in the ROC plot of the multivariable model was 0.714 (0.619–0.809) (Fig. 3B).

Multivariable Logistic Regression Analysis for Intraoperative Bleeding Exceeding 30% of the Total Body Blood Volume
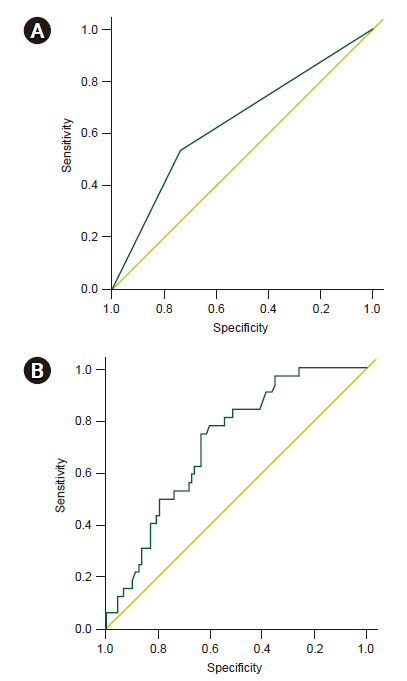
Receiver operating characteristic plot of the categorized cephalhematoma size (A), and of the multivariable model (B). Area under the curve: 0.635 (0.536–0.734) and 0.714 (0.619–0.809), respectively.
DISCUSSION
This study showed that cephalhematoma size measured in the preoperative CT images was linearly correlated with intraoperative blood loss. Furthermore, multivariable logistic regression analysis revealed that a cephalhematoma size greater than 113.5 cm3 was an independent risk factor for large blood loss during cranioplasty.
One of the most common causes of cardiac arrest during pediatric surgery is hypovolemia due to intraoperative bleeding, and it often occurs in craniofacial surgery [8]. Therefore, meticulous fluid management is required for hemodynamic stability and maintenance of major organ perfusion in cranioplasty for children. Thus, clinicians are recommended to use estimates of total blood volume to determine transfusion needs during pediatric craniofacial surgery [6]. In our study, the overall incidence of intraoperative hypotension was 88.33%, and in terms of the incidence of severe hypotension, the patients in the large blood loss group were hemodynamically more unstable than those in the small blood loss group. As most of the patients in our study population were healthy without any underlying medical comorbidities and since hypotension did not occur during the induction of general anesthesia but occurred during surgery, surgical bleeding was considered the main cause of hypotension in this study. Considering that the mean surgery duration was 71.2 min, a large amount of bleeding occurred in a short period, making hemoglobin-based transfusion difficult. While bleeding occurs in a short duration, confirming the hemoglobin level in the arterial blood gas analysis takes time. Therefore, as regards intraoperative fluid and transfusion management, identifying risk factors that can predict large blood loss based on the total body blood volume and implementing a transfusion strategy prior to surgery would be clinically useful for anesthesiologists. Cephalhematoma size larger than 113.5 cm3 was found to be the most important risk factor for large blood loss which anesthesiologists should carefully check before surgery. In addition to the cephalhematoma size, age was another independent risk factor for large blood loss presumably due to the technical difficulty of surgery at an older age [3,4].
ImageJ, which we used to measure the size of the cephalhematoma, is a Java-based software for image processing developed at the National Institute of Health [9]. The accuracy of manual volumetry performed by clinicians using ImageJ on a personal computer was reported in a previous study based on hepatic CT [10]. Additionally, another previous study performed manual volumetry using ImageJ to quantify deep gray matter in the brains of infants [11]. Therefore, developing a transfusion strategy prior to pediatric cranioplasty using cephalhematoma size measured by ImageJ may be helpful in maintaining hemodynamic stability during surgery.
In previous randomized trials based on pediatric postsurgical patients [12,13], a restrictive transfusion strategy showed no increase in mortality and multiorgan dysfunction when compared with a liberal transfusion strategy. The mean age of the patients in these randomized trials varied from 26.4 to 73.7 months. Maintaining hemoglobin levels ≥ 8 g/dl was recommended as the standard in patients with massive bleeding during surgery [6,14,15]. However, even in adult patients, complicated hemorrhage—defined as hemorrhage exceeding 30% of the total body blood volume—almost always causes signs of hypoperfusion such as hypotension and tachycardia [16,17]. Transfusion is usually required for this substantial blood loss [16]. In general, massive blood loss in acute situations is defined as blood loss of more than 50% of the total body blood volume within a period of 3 h [18,19]. Considering that the mean age of the patients in this study was 4.5 months, blood loss exceeding 30% of the total body blood volume within a mean surgery duration of 71.2 min almost always requires blood transfusion.
On the contrary, the initial postoperative hemoglobin level confirmed in the general ward or neurological intensive care unit was higher in the large blood loss group than in the small blood loss group, which appeared to be related to the larger transfusion volumes required in the large blood loss group than in the small blood loss group. The short duration of massive transfusion is known to be a risk factor for over-transfusion [20]. However, an initial postoperative hematocrit level > 30% was reported to reduce the risk of postoperative red blood cell transfusion in pediatric patients undergoing craniofacial surgery [21]. Moreover, no patients in our study experienced over-transfusion-related complications, such as infection, transfusion-related acute lung injury, or circulatory overload [22].
This study has some limitations. First, as this retrospective study was based on electronic medical records, performing a prospective study would be helpful in confirming a more accurate cutoff value for cephalhematoma size to facilitate transfusion management. Second, this study was based on data from a single center that was analyzed by two surgeons; additionally, intraoperative blood loss may be surgeon dependent. Thus, this result cannot be universally applicable to cranioplasty performed by other surgeons in different institutions. Third, the intraoperative transfusion in this study was performed without confirmation of the hemoglobin level in the event of massive blood loss causing hemodynamic instability. Thus, the correlation between the cephalhematoma size and amount of packed red blood cell transfused cannot be determined based on this retrospective study in which transfusion was performed without laboratory confirmation.
In conclusion, the cephalhematoma size measured in the preoperative CT images is an independent risk factor for blood loss exceeding 30% of total body blood volume. Thus, we recommend implementing a transfusion strategy prior to pediatric cranioplasty based on cephalhematoma size measured by ImageJ as a new clinical model for intraoperative transfusion management.
Notes
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
DATA AVAILABILITY STATEMENT
The datasets generated during and/or analyzed during the current study are not publicly available but are available from the corresponding author on reasonable request.
AUTHOR CONTRIBUTIONS
Conceptualization: Seung Hyun Kim, Kyeong Tae Min, Seung Ho Choi. Data acquisition: Seung Hyun Kim, Kyeong Tae Min, Eun Kyung Park, Hyungjin Rhee, Hyukjin Yang, Seung Ho Choi. Formal analysis: Seung Hyun Kim, Seung Ho Choi. Writing – original draft: Seung Hyun Kim, Seung Ho Choi. Writing – review and editing: Seung Hyun Kim, Kyeong Tae Min, Eun Kyung Park, Hyungjin Rhee, Hyukjin Yang, Seung Ho Choi.