Hypertrophic osteoarthropathy in renal cell carcinoma - A case report -
Article information
Abstract
Background
Hypertrophic osteoarthropathy (HOA) is a rare clinical condition including an abnormal periosteal reaction in the long bones that causes painful swelling and tenderness of the extremities, digital clubbing, arthritis, synovitis, and joint effusions. Most cases are associated with tumorous conditions and most commonly with lung cancer. HOA has been rarely reported in association with other cancers.
Case
A patient with a history of recurrent renal cell carcinoma was referred to our clinic with bilateral leg pain, knee joint effusion, and arthritis. Simple radiography and bone scintigraphy confirmed a diagnosis of HOA. Oral non-steroidal anti-inflammatory drugs, joint fluid aspiration, and intra-articular injection of pain medications were found to be effective in the management of HOA pain.
Conclusions
HOA prognosis depends on the underlying disease, therefore, cancer treatment is critical. This case demonstrates the need to consider HOA in patients with various malignancies who present with bone or joint pain of the extremities.
Hypertrophic osteoarthropathy (HOA) is a rare clinical condition including an abnormal periosteal reaction of the long bones that causes painful swelling and tenderness of the extremities, digital clubbing, arthritis, synovitis, and joint effusions [1]. Primary HOA is an autosomal dominant hereditary disease and represents only 3% of all cases [2]. Secondary HOA is predominantly associated with tumorous conditions and primarily with lung cancer [3]. HOA has been rarely reported as a paraneoplastic syndrome associated with various malignancies including gastrointestinal, hematologic, nasopharyngeal, melanoma, breast, and renal cell cancer [3,4]. In one study, only two out of 30 patients presented with HOA caused by renal cell cancer (6.7%) [4]. Here, we review the diagnosis and treatment of an atypical case of HOA in a patient with recurrent renal cell cancer.
CASE REPORT
The patient was informed and has provided written consent for the publication of this case report.
A 53 year old man was referred to our pain clinic for painful bilateral lower leg swelling, which began 1 month earlier. On presentation, his pain severity was 6–8/10 on the visual analogue scale (VAS). He had a past medical history of renal cell carcinoma diagnosed 3 years ago and radical nephrectomy of the left kidney. After 1 year, he was found to have recurrent renal cell carcinoma and underwent chemotherapy. Moreover, he underwent a left hemicolectomy 1 year ago because of a metastatic lesion in the descending colon.
Physical exam revealed fluid shifting, tender swelling, and painful limitation of range of motion of both knees, suggesting joint effusion (Fig. 1). Digital clubbing was not present. To find the cause of the painful lower leg swelling, simple radiologic studies from the pelvis to the feet and whole body bone scintigraphy with Tc-99m hydroxymethylene diphosphonate were performed. Periosteal reactions were observed in both tibias, fibulas, and femurs on simple radiologic studies (Fig. 2). Bone scintigraphy revealed increased radiotracer uptake along the cortex of the appendicular bones (Fig. 3). Although the digital clubbing was not present, we could diagnose hypertrophic osteoarthropathy based on periosteal reactions found on X-rays and bone scintigraphy.
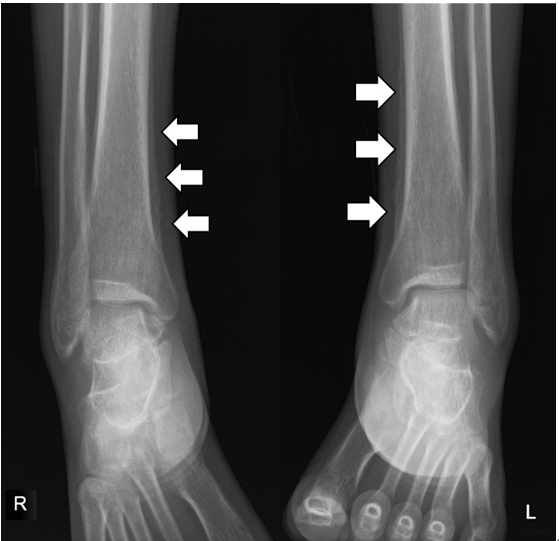
Simple radiologic studies of the patient’s feet. A bilateral periosteal reaction indicates hypertrophic osteoarthropathy (arrows).

Whole body bone scintigraphy. Increased radiotracer uptake is observed along the appendicular bone cortex.
The patient was prescribed naproxen 1,000 mg/d for pain. An ultrasound guided therapeutic arthrocentesis of both knees was performed. Clear, yellowish joint fluid was aspirated from both knees (right 4 ml, left 12 ml). After the arthrocentesis, both knees were intra-articularly injected with a mixture of 1 ml ropivacaine, 0.75 mg/ml; 2 ml sodium hyaluronate, 10 mg/ml; triamcinolone acetonide 10 mg; and morphine sulfate 0.5 mg.
At 1-week follow-up, the pain was greatly reduced from VAS 6–8/10 to 1–2/10. At the patient’s request, another ultrasound guided therapeutic arthrocentesis was performed, with 2 ml and 3 ml of joint fluid aspirated from the right and left knee, respectively. Subsequently, a mixture of 1 ml ropivacaine, 0.75 mg/ml; 2 ml sodium hyaluronate, 10 mg/ml; triamcinolone acetonide 10 mg; and morphine sulfate 1 mg was injected in each knee joint. The patient showed no side effects after arthrocentesis and injection.
The patient is undergoing chemotherapy for treatment of his renal cell cancer. Non-steroidal anti-inflammatory drugs (NSAIDs) are recommended for pain control. At the last follow-up, four months since the original arthrocentesis, the patient reported his pain level as VAS 1–2/10.
DISCUSSION
HOA is a syndrome clinically characterized by abnormal skin and periosteal proliferation of the distal extremities [1]. Patients with HOA may be asymptomatic or present various clinical signs. The classical triad for HOA is digital clubbing, periostosis, and synovial effusions. Patients often present with periostosis, although not all patients have digital clubbing, joint pain, or effusion [5]. Patients may feel a burning sensation and bone pain as the disease progresses [1]. Clinical diagnosis may be challenging because the symptoms are similar to those of connective tissue diseases or inflammatory arthritis. In this case, the patient showed clinical signs of periostosis as pain and swelling of both legs and joint effusion of both knees but did not have clubbing of the fingers or toes.
The mechanism of pathogenesis of HOA is unclear. One possibility is a neurogenic pathway model. The vagus nerve innervates the organ with disease and induces a neural reflex that may cause vasodilation followed by increased blood flow to the extremities [6]. Another possibility is a humoral pathway. Hypoxia in patients with lung disease induces cytokines and growth factors such as vascular endothelial growth factor (VEGF), platelet-derived growth factor, and prostaglandin E2 (PGE2). These molecules induce development of new periosteal bone formation [7].
Primary HOA is a rare hereditary disease representing only 3% of all cases of HOA [2]. Also known as pachydermoperiostosis, it is characterized by early onset of clubbing and thickening of the skin of the face. Primary HOA involves mutations of the 15-hydroxyprostaglandin dehydrogenase gene and the solute carrier organic anion transporter family member 2A1 gene. Mutation of these genes impairs the ability to degrade PGE2. Elevation of PGE2 results in overexpression of VEGF. In consequence, excessive new bone formation appears by osteoblasts [8].
Secondary HOA is primarily associated with abnormal lung function because of lung cancer, interstitial lung disease, sarcoidosis, chronic obstructive pulmonary disease, pulmonary infections, abscess, empyema, or mesothelioma. Even with undamaged lungs, cyanotic heart disease can cause HOA by excluding the lungs from systemic circulation [1,3]. The most common cause of secondary HOA is non-small cell lung cancer. The incidence of HOA in lung cancer is reported as 4% to 17% [5]. It may appear as a generalized or localized form involving only one or two extremities. The generalized form is caused by systemic disease, while the localized form is associated with endothelial injury, such as arterial aneurysm, arterial graft infection, or a functioning arteriovenous fistula [9]. HOA has been rarely reported as a paraneoplastic syndrome in other malignancies including gastrointestinal, hematologic, nasopharyngeal, melanoma, breast, and renal cell cancer [3,4]. Renal cell cancer was the cause of HOA in this case.
Imaging evaluation can be a major tool for diagnosing HOA because serological tests are not reliable [3]. Plain radiographs are used as the first modality. Periostosis along the shaft of tubular bones is the key feature found on plain radiographs. The most commonly affected bones are the tibia, fibula, radius and ulna [3]. They may also present bony deformities and soft tissue swelling. Long standing clubbing can result in osseous resorptions of the fingers and toes. These bony changes appear first in the toes before they manifest in the fingers [1]. Joint involvement can also appear on plain radiographs as synovial effusions, joint space narrowing, erosions, or periarticular osteopenia [3].
Magnetic resonance imaging (MRI) can also be used to show periosteal reactions, osseous proliferation at the ligaments and tendons in later stages, and specific soft tissue changes in periarticular swelling sites. Also, MRI can be useful for identifying synovial effusion [3,10].
Bone scintigraphy is more sensitive for detecting HOA than radiography alone [11]. Patients with known malignancies are often found to have HOA on bone scintigraphy [3]. Significant radiotracer uptake is shown at the periosteum along the cortical margin of long tubular bones [12]. This modality can be used to estimate the response to therapy if findings resolve after treatment [13]. Similar to bone scintigraphy, positron emission tomography with 18F isotopes can also be used to show the hypermetabolic activity along the long tubular bones. In this case, periosteal reactions observed on simple radiologic studies and bone scintigraphy were diagnostic for HOA.
Radiological signs of periosteal reactions can appear in various conditions including thyroid acropachy, leukemia, lymphoma, hypervitaminosis A, venous stasis, and use of medications such as voriconazole. The type and distribution of periosteal reaction varies in these conditions. Bilaterally symmetrical involvement of the appendicular skeleton characterizes HOA [1,3]. Identifying underlying disease and reviewing medical history may help in patient diagnosis and treatment. In this case, the patient had known renal cell cancer, an absence of thyroid diseases, hematologic malignancies, or venous insufficiency, and no use of retinoids or voriconazole.
Because the prognosis and mortality of secondary HOA are associated with underlying disease, treatment should be focused on the primary disease, even considering surgical resection of the primary tumor. Symptomatic treatment options include analgesics, such as NSAIDs. In some cases, bisphosphonate and octreotide provided effective symptomatic treatment of bone pain [14]. Also, truncal vagotomy has shown symptomatic relief for refractory patients [15]. In this case, aspiration of knee joint fluid and intra-articular injection for pain were found to be effective. The patient is undergoing chemotherapy for the renal cell cancer after surgery on the primary and colon metastasis sites.
In summary, this case demonstrates that HOA should be considered in patients with malignancies other than lung cancer when they have bone or joint pain of the extremities, even without digital clubbing. Treating the underlying disease and pain management are both important. Pain management options in patients with HOA include analgesic medications such as NSAIDs, bisphosphonate, octreotide, surgery of the original tumor, and sympathectomy. As in this case, joint aspiration and intra-articular injection can be a treatment option for patients with joint effusions.
Notes
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
DATA AVAILABILITY STATEMENT
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
AUTHOR CONTRIBUTIONS
Conceptualization: Hwa-Yong Shin. Writing - original draft: Kyung Seo Oh. Writing - review & editing: Kyung Seo Oh, Seung Young Lee, Hwa-Yong Shin. Supervision: Se-Hee Min, Choongun Ryu, Hwa-Yong Shin.

