Approaching trauma analgesia using prolonged and novel continuous peripheral nerve blocks - A case report -
Article information
Abstract
Background
A supraclavicular brachial plexus nerve block provides analgesia for the shoulder, arm, and hand; however, the maximum safe duration for a continuous infusion remains controversial. A novel continuous peripheral nerve block (CPNB) technique combining the Lateral, Intermediate, and Medial femoral cutaneous nerves (termed the ‘LIM’ block) to provide analgesia to the lateral, anterior, and medial cutaneous areas of the thigh while preserving quadriceps strength will also be described in detail here.
Case
We present a complex case in which simultaneous utilization of an unilateral supraclavicular CPNB (5 weeks) and bilateral LIM CPNB (5 days) are successfully performed to provide analgesia for a traumatic degloving injury resulting in multiple surgeries.
Conclusions
The analgesic plan in this case study eliminated previous episodes of opioid-induced delirium, facilitated participation in recovery, and removed concerns for respiratory depression and chronic opioid use in a patient at particular risk for both issues.
Traumatic injuries often cause significant acute pain, intensified by required surgeries and painful dressing changes. The amalgamation of complicated injuries and pain intensity requires complex analgesia to achieve adequate pain control. Prolonged healing time, combined with opioid-centric analgesia regimens expose patients to harmful, potentially avoidable, opioid-related adverse drug events (ORADEs) [1].
Continuous peripheral nerve blocks (CPNB) carry proven advantages in the setting of acute traumatic and post-surgical pain, including improved provision of analgesia and reduced ORADE’s [2]. Post-intervention immobility is a disadvantageous limitation of some CPNB techniques such as the fascia iliaca block due to the decrease in quadricep muscle strength and resulting increased risk in patient falls [3]. Further, the maximum safe duration for a continuous infusion remains controversial [4]. Herein, the authors present a case of simultaneous, continuous, and prolonged analgesia by employing a supraclavicular CPNB combined with a novel CPNB technique which provides continuous cutaneous analgesia to the thigh, while preserving motor strength and facilitating productive physical and occupational therapy sessions.
CASE REPORT
The patient provided written informed consent for publication of this case report and the associated images.
A 76-year-old male patient sustained injuries that included a comminuted left humerus midshaft fracture and a thermal contact abrasion with full thickness burns and degloving of the left shoulder, upper arm, and extensor surface of the lower arm and hand. His past medical history was significant for obesity, obstructive sleep apnea, type 2 diabetes mellitus, hypertension, and gastroesophageal reflux disease.
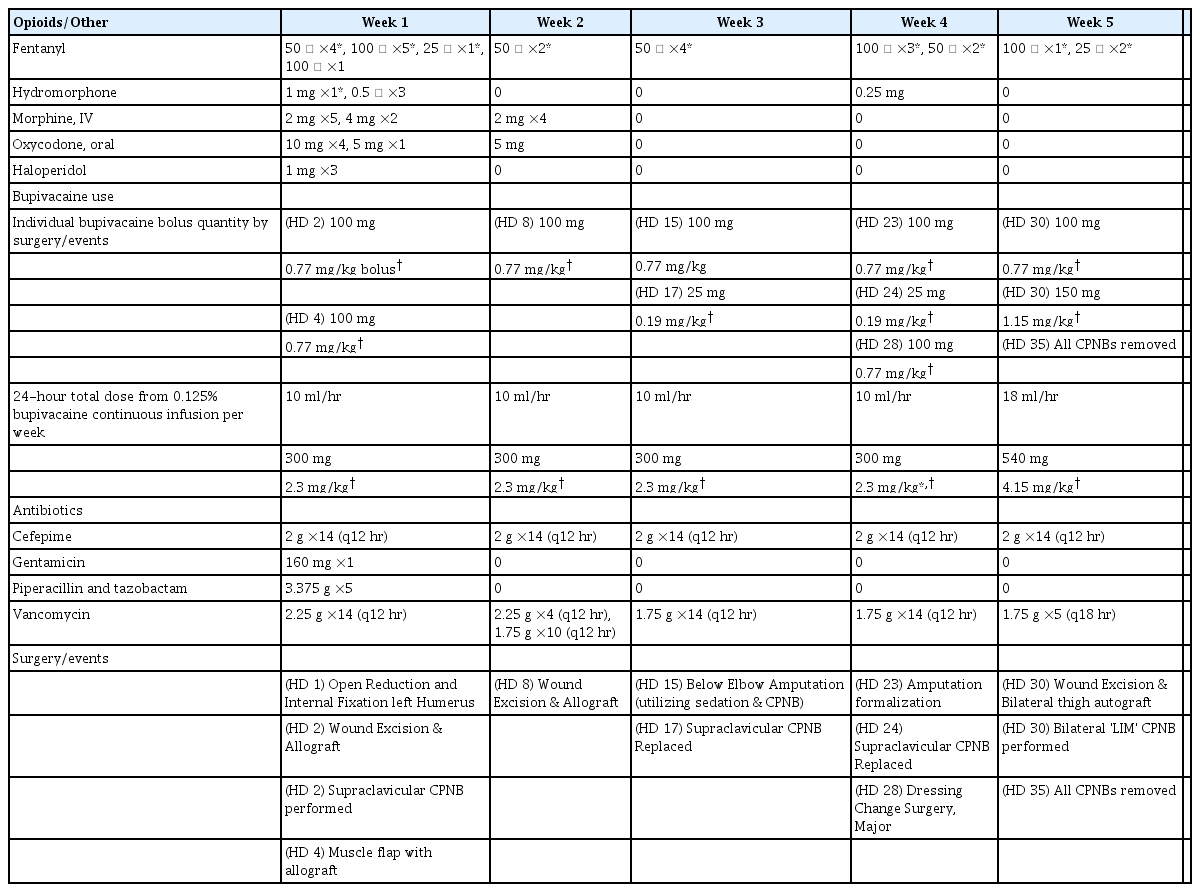
The patient immediately underwent an open reduction and internal fixation of the left humerus, followed by burn wound excision and application of allograft to the left upper extremity. Pain intolerance with dressing changes and opioid-associated delirium prompted an Acute Pain Service (APS) consultation. Accordingly, APS performed an ultrasound-guided, left supraclavicular CPNB (B Braun Contiplex Needle, B-Braun Medical Inc., USA) using 20 ml of 0.5% bupivacaine followed by a 10 ml/h continuous infusion of 0.125% bupivacaine through an electronic infusion pump (CADD Solis infusion system, Smiths Medical, USA). Analgesia dramatically improved, and symptoms of delirium abated in parallel to reduced opioid consumption (Table 1). Prior to each of the remaining 7 surgeries performed under general anesthesia, APS bolused the supraclavicular CPNB with 20 ml of 0.5% bupivacaine.
Thereafter, the patient underwent a below elbow amputation on hospital day (HD) 15. The supraclavicular CPNB was utilized as the primary anesthetic along with intravenous propofol sedation and replaced on HD 17. Amputation formalization occurred on HD 23, and APS carried out routine exchange of the supraclavicular CPNB catheter on HD 17 and HD 24 to reduce the potential risk for catheter site infection.
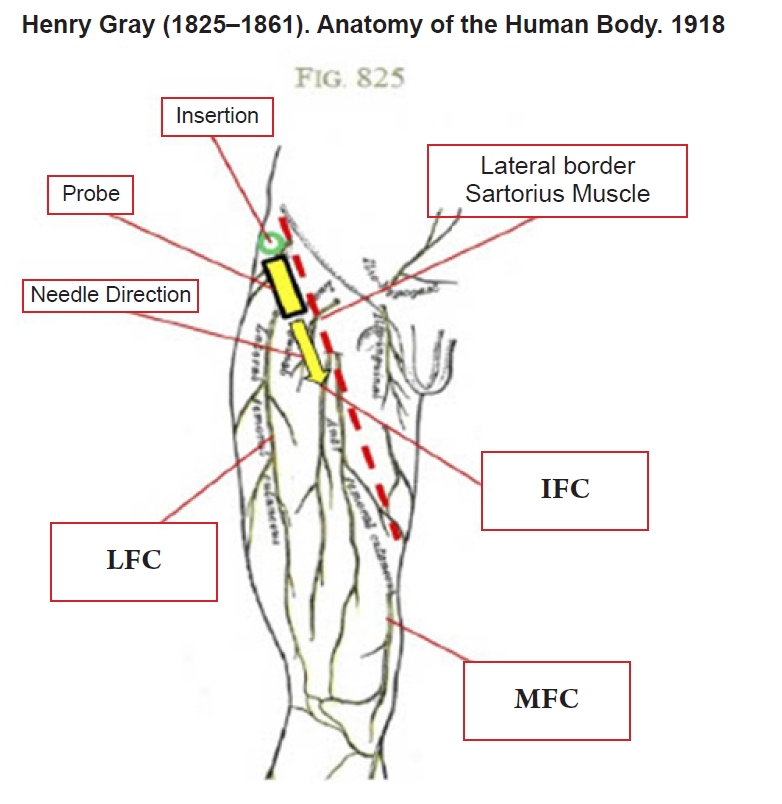
The patient then underwent a burn wound excision of the left arm and received an extensive split thickness skin graft (1,140 cm2) from both thighs on HD 30. For donor site analgesia and to further mitigate opioid-induced delirium, APS performed an ultrasound-guided bilateral Lateral, Intermediate, and Medial femoral cutaneous nerves (LIM) CPNB intraoperatively using a total of 40 ml of 0.375% bupivacaine. The novel LIM CPNB technique was performed by directing the needle caudally and medially above the fascia iliaca along the lateral border of the sartorius muscle. The sartorius muscle serves as an anatomical landmark as the lateral femoral cutaneous nerve enters the thigh lateral to the sartorius muscle near the LIM block insertion site. The intermediate and medial cutaneous branches of the femoral nerve respectively supply anterior and medial cutaneous thigh sensation and pierce the fascia iliaca just lateral to the sartorius muscle distally. Hydrodissection with local anesthetic allows the needle to advance easily in the correct plane just above the fascia iliaca. Ultrasound and anatomy images describe the nerve block procedure and relevant sonoanatomy (Figs 1–4) [5].
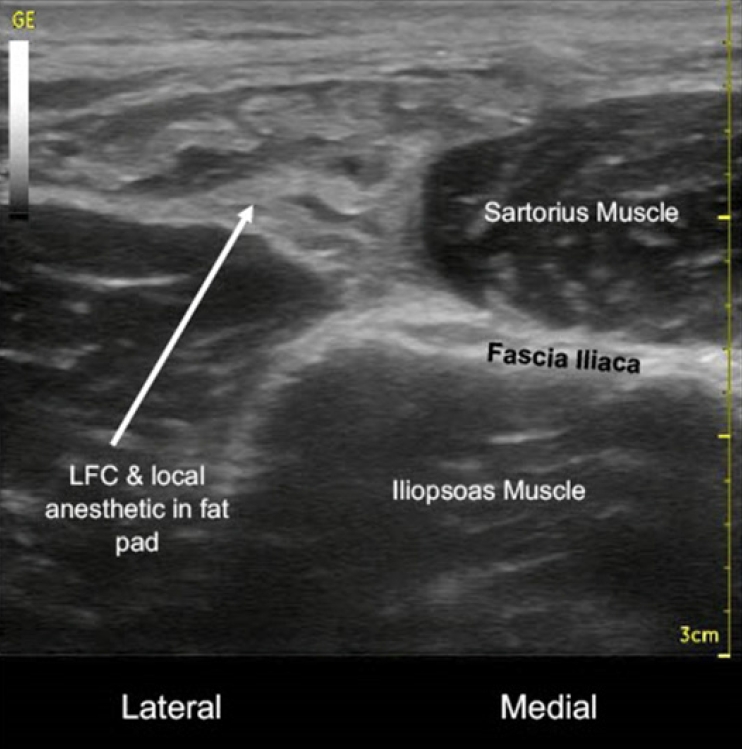
Lateral femoral cutaneous (LFC) nerve & local anesthetic in fat pad over fascia iliaca and iliopsoas muscle lateral to sartorius muscle with probe in transverse view (post-block).
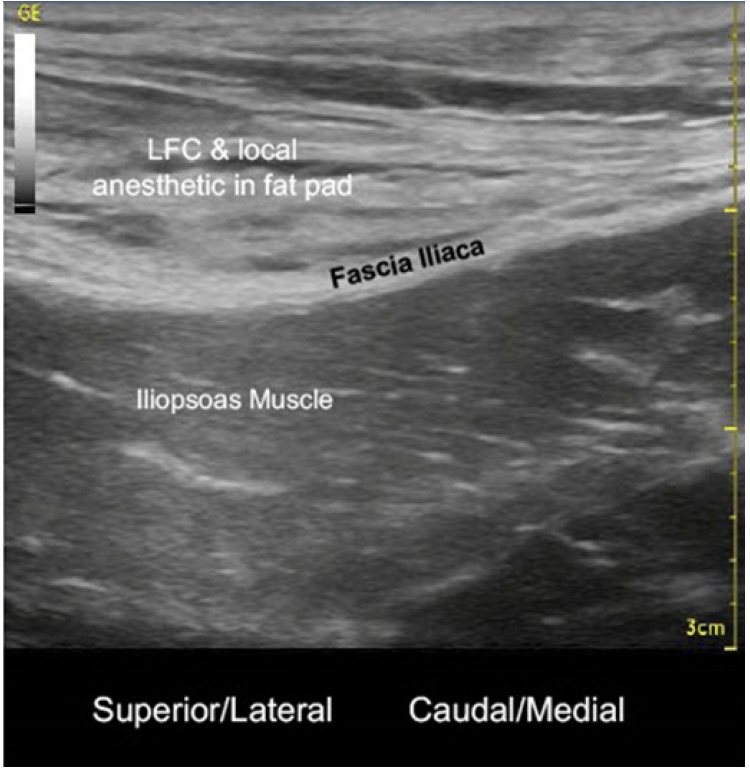
Lateral femoral cutaneous (LFC) nerve & local anesthetic in fat pad over fascia iliaca and iliopsoas muscle lateral to sartorius muscle with probe in near sagittal view (post-block).
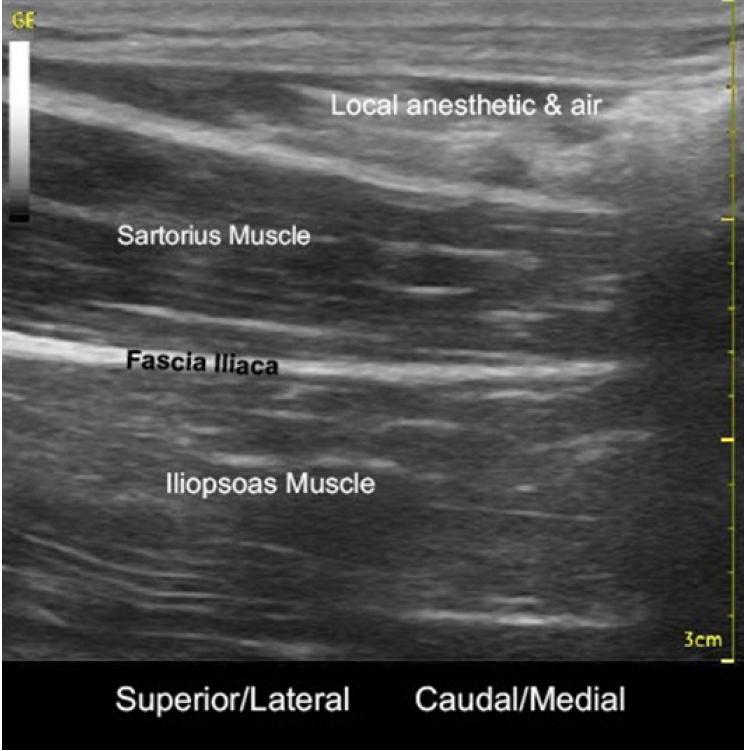
Local anesthetic & air seen tracking medially above sartorius muscle in near sagittal view (post-block).
For the next 5 days, APS continuously infused a total of 8 ml/hr of 0.125% bupivacaine through a second electronic infusion pump utilizing a catheter tubing splitter (6 inch Bifurcated Blue Stripe Extension, ICU medical, USA) to the LIM blocks. On HD 35, APS held the supraclavicular and LIM block infusions to evaluate for remaining underlying pain. After confirming adequate analgesia without requirements for opioids, APS removed all three CPNB catheters without complication or evidence of infection.
DISCUSSION
The authors report this complex case demonstrating the successful use of a continuous unilateral supraclavicular nerve block for 5 weeks for ongoing left upper extremity pain supplemented with a novel LIM CPNB technique performed to control pain in the lateral, anterior, and medial cutaneous portions of both thighs. This comprehensive regional analgesic approach helped control postoperative pain, reduce opioid consumption, and facilitate therapy participation.
Throughout the 5-week supraclavicular CPNB infusion, the patient confirmed adequately controlled pain, utilizing only scheduled acetaminophen and requiring minimal opioids (Week 1 [prior to CPNB]: 159 oral morphine milligram equivalents [MME]; Week 2–5 average weekly oral MME: 8.88) for pain despite several painful surgeries, dressing changes, and participation with physical and occupational therapy. The patient exhibited no signs of local infection, local anesthetic systemic toxicity (LAST), and no evidence of residual weakness or numbness to the left arm. Throughout the 5-day continuous LIM block infusion, the patient denied thigh tenderness to palpation. Physical examination by APS demonstrated decreased temperature sensation to the lateral, anterior, and medial thigh and bilateral 5/5 strength of quadriceps each day. Consequently, the patient remained able to participate in physical and occupational therapy with LIM block infusions and without limitation due to quadriceps weakness or pain.
Adequate pain control facilitates earlier ambulation and discharge, improves functional recovery, and helps prevent other consequences of traumatic amputation, such as phantom and residual limb pain [6]. Utilization of long-term CPNB can reduce the risk of chronic post-surgical pain and mitigate downstream effects of prolonged exposure to opioids and related ORADEs, such as post-operative respiratory insufficiency, opioid dependence, and opioid-induced delirium experienced by this patient [7]. Patients suffering severe traumatic injuries are at risk for prolonged opioid exposure and, ultimately, opioid dependence [1]. This patient presented with a high risk for multiple ORADEs, given his past medical history and sustained trauma.
Significant aspects of the LIM CPNB for thigh autograft pain include requiring a relatively low bupivacaine infusion rate to reduce the risk for developing LAST and preserving quadricep muscle strength to lower the risk of falls. Furthermore, the combined LIM CPNB consisting of the lateral, intermediate, and medial femoral cutaneous nerves performed in a single block provided reliable analgesia for the lateral, anterior, and medial cutaneous regions of both thighs. The anterior femoral cutaneous nerve, which carries the intermediate and medial femoral cutaneous nerves, additionally supplies cutaneous analgesia to the anteromedial knee [8]. In contrast to the novel technique described herein, other CPNB techniques traditionally utilized to control pain from thigh autograft harvesting, such as the femoral or fascia iliaca nerve blocks, produce quadriceps weakness and can lead to the common complication of patient falls [3]. The combined CPNBs provided an efficacious, alternative approach for analgesia, while promoting patient safety and participation in therapy.
Infection remains one of many concerns with CPNBs and has been associated with duration of catheter use [9]. Though the patient’s requirement for antibiotics (Table 1) helped reduce the local infection due to prolonged catheter utilization risk, clinicians must keep the infection concern in mind during treatment. Many clinical practices have evolved by including the routine use of chlorhexidine skin preparation and cyanoacrylate glue for catheter site entry [4]. A specific recommendation regarding the duration of epidural or CPNB catheterization that is associated with an increased risk of infectious complications has not been issued, and studies have demonstrated minimal evidence of CPNB catheter-related infections despite prolonged use [10].
Concerns regarding nerve injury risk while replacing CPNBs with partially anesthetized nerves are valid, but ultrasound guidance and clinical experience mitigate this risk [11]. Given the extended infusion of CPNBs in this case, clinicians should consider the risk of LAST [12]. As standard practice, total daily local anesthetic usage is carefully calculated, and patients are continually monitored and verbally screened for LAST every 6 hours. As a final mitigation strategy, nurses maintain APS generated annual competencies for managing patients receiving CPNB.
While these risks are not trivial, the short and long-term risks associated with extended opioid exposure remain significant and should equally be considered [1,7]. Post-operative pain management with opioids independently serves as a risk factor for chronic opioid use even in opioid naïve patients [1,2]. This patient’s injuries required multiple surgeries and would have required multiple weeks of escalating opioid doses.
Anesthesiologists involved in trauma and burn injuries could consider these techniques, particularly for patients with risk factors for addiction and ORADEs. Further investigation is needed to examine the risks and benefits of prolonged CPNBs and dressing management protocols in trauma patients. Evaluating optimal dosing for initial LIM block boluses and infusion rates, the risks and benefits of single injection and continuous LIM blocks versus fascia iliaca blocks or lateral femoral cutaneous blocks for thigh autografts are needed. Given the utilization of multiple CPNB, uncertainty arises regarding the efficacy and practicality of such approaches outside the trauma setting.
This case study demonstrates successful, prolonged usage of a supraclavicular CPNB in a patient with complex injuries. Further, the authors demonstrate a novel LIM CPNB requiring less anesthetic and providing extensive analgesia for bilateral thigh autografts while maintaining quadriceps strength. The analgesic plan in this case study eliminated previous episodes of opioid-induced delirium, facilitated participation in recovery, and removed concerns for respiratory depression and chronic opioid use in a patient at particular risk for both issues.
Acknowledgements
Figs. 1–3 courtesy of Jerry Jones, MD.
Notes
FUNDING
None.
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
DATA AVAILABILITY STATEMENT
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
AUTHOR CONTRIBUTIONS
Conceptualization: Eric Ly, Jerry Jones. Formal analysis: Jerry Jones. Methodology: Ban Tsui. Investigation: Jerry Jones. Supervision: Ban Tsui, Jerry Jones. Validation: Jerry Jones. Writing - original draft: Eric Ly, Jerry Jones. Writing - review & editing: Eric Ly, Sai Velamuri, William Hickerson, David M. Hill, Jay Desai, Ban Tsui, Michael Herr, Jerry Jones.