 |
 |
- Search
| Anesth Pain Med > Volume 17(1); 2022 > Article |
|
Abstract
Background
Methods
Results
Notes
DATA AVAILABILITY STATEMENT
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
AUTHOR CONTRIBUTIONS
Conceptualization: Sung Mi Ji, Min A Kwon. Formal analysis: Min A Kwon. Methodology: Min A Kwon. Writing - original draft: Jae Gyok Song, Nayoung Choi. Writing - review & editing: Min A Kwon. Investigation: Jae Gyok Song, Nayoung Choi, Minji Kang, Min A Kwon. Resources: Sung Mi Ji, Dong-wook Kim. Software: Minji Kang. Supervision: Dong-wook Kim, Min A Kwon.
Fig. 2.

Fig. 3.
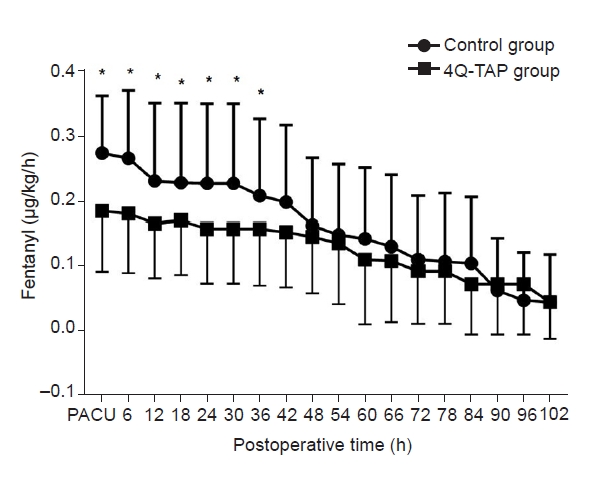
Table 1.
All measured values are presented as number only, mean ± SD, or number (%). M/F: male/female, 4Q-TAP: four-quadrant transabdominal plane, ASA: American Society of Anesthesiologists, CC: completeness of cytoreduction, PCI: peritoneal carcinomatosis index, PONV Hx: History of Postoperative Nausea and Vomiting. The Apfel simplified score includes female sex, history of PONV and/or motion sickness, non-smoking status, and postoperative use of opioids. When 0, 1, 2, 3, or 4 factors are present, the risk of PONV is 10, 20, 40, 60, or 80% respectively [12]. PCI is a diagnostic and prognostic tool that is the sum of the scores of 13 abdominal regions. Each region is assigned a score of 0-3 based on the largest tumor size in each region. The scores ranged from 0 to 39. Higher scores indicated more widespread and/or larger tumors in the peritoneal cavity. The CC score is an assessment of residual disease after maximal surgical cytoreduction. According to the size of the residual tumor, the score is graded with CC0 (none), CC1 (< 2.5 mm), CC2 (2.5-25 mm), or CC3 (> 25 mm) [13].
Table 2.
| Variable | Control (n = 33) | 4Q-TAP (n = 36) | P value |
|---|---|---|---|
| Duration of operation (min) | 474.2 ± 177.7 | 457.3 ± 160.1 | 0.680 |
| Duration of anesthesia (min) | 538.4 ± 184.7 | 533.5 ± 155.3 | 0.906 |
| Propofol (mg) | 2,756.2 ± 1,170.3 | 3,066.1 ± 1,540.2 | 0.547 |
| Remifentanil (mg) | 2,875.0 ± 1,674.0 | 2,825.0 ± 1,978.5 | 0.358 |
| Intraoperative fluid (ml) | 6,485.2 ± 3,471.6 | 5,151.7 ± 2,257.0 | 0.061 |
| Urine output (ml) | 1,450.0 ± 1,067.0 | 1,318.7 ± 1,022.7 | 0.585 |
| Estimated blood loss (ml) | 400 (200, 1,500) | 350 (200, 600) | 0.039* |
| Transfusion (%) | 13 (39.4) | 12 (33.3) | 0.601 |
Table 3.
Table 4.
REFERENCES
-
METRICS

-
- 3 Crossref
- 3,757 View
- 89 Download
- Related articles in Anesth Pain Med
- ARTICLE & TOPICS
-
- Topics
-
- Neuroscience in anesthesiology and critical care
- Anesthetic Pharmacology
- Obstetric Anesthesia
- Pediatric Anesthesia
- Cardiothoracic and Vascular Anesthesia
- Transplantation Anesthesia
- Spinal Pain
- Regional Anesthesia
- Neuromuscular Physiology and Pharmacology
- Airway Management
- Geriatric anesthesia and Pain
- Others








