Retrospective analysis of the feasibility and safety of external jugular vein cannulation in surgical patients
Article information
Abstract
Background
Establishing intravenous (IV) access is an essential procedure in surgical patients. External jugular vein (EJV) cannulation can be a good alternative for patients for whom it is difficult to establish peripheral IV access. We aimed to investigate the feasibility and safety of EJV cannulation in surgical patients.
Methods
We performed a retrospective review of EJV cannulation in patients who underwent anesthesia for surgery at a tertiary hospital between 2010 and 2021. We collected clinical characteristics, including EJV cannulation-related variables, from the anesthetic records. We also investigated the EJV cannulation-related complications, which included any EJV cannulation-related complications (insertion site swelling, infection, thrombophlebitis, pneumothorax, and arterial cannulation) within 7 days after surgery, from the electronic medical records during the hospitalization period for surgery.
Results
We analyzed 9,482 cases of 9,062 patients for whom EJV cannulation was performed during anesthesia. The most commonly performed surgery was general surgery (49.6%), followed by urologic surgery (17.5%) and obstetric and gynecologic surgery (15.7%). Unplanned EJV cannulation was performed emergently during surgery for 878 (9.3%) cases. The only EJV cannulation-related complication was swelling at the EJV-cannula insertion site (65 cases, 0.7%). There was only one case of unplanned intensive care unit admission due to swelling related to EJV cannulation.
Conclusions
Our study showed the feasibility and safety of EJV cannulation for surgical patients with difficult IV access or those who need additional large-bore IV access during surgery. EJV cannulation can provide safe and reliable IV access with a low risk of major complications in a surgical patient.
INTRODUCTION
Establishing peripheral intravenous (IV) access is essential for surgical patients for the administration of medications, fluids, and blood products during the perioperative period. However, obtaining reliable peripheral IV access in some patients can be challenging such as those with obesity and a history of IV drug abuse, as well as those who have received chemotherapy via peripheral cannula, frequent IV cannulation, and dialysis [1,2]. Central venous catheterization (CVC) can provide reliable venous access; however, it is more difficult than peripheral IV cannulation and can have severe complications such as thrombosis, pneumothorax, and infection [3,4].
The external jugular vein (EJV) is a superficial central vein located away from major neurovascular structures with less anatomical variation than other central veins [5,6], possibly accounting for the lower risks of major complications after EJV cannulation relative to those noted with other central vein cannulations [7,8]. Additionally, the EJV is more visible than other central veins and located closer to the heart than peripheral veins [9]. Therefore, EJV cannulation has been used in patients with difficult IV access mainly in emergency medicine [1,10]. EJV cannulation can be also a good alternative for surgical patients in whom it is difficult to establish peripheral IV access. If it is difficult to access peripheral veins due to the surgical drape or proximity to surgical site, EJV can be relatively easily accessible intraoperatively except for head and neck surgeries. EJV was also proposed as an alternative to other central venous access in patients with severe coagulopathy or in cases where ultrasound is not available [5,11].
For these reasons, EJV cannulation has been commonly performed by anesthesiologists for surgical patients with difficult IV access in our institution. However, its feasibility and safety for surgical patients has been scarcely reported. Therefore, we aimed to retrospectively analyze its feasibility and safety using the data of surgical patients in our institution over the past 12 years.
METHODS
Study design
We performed a retrospective review of EJV cannulation in surgical patients at a tertiary care teaching hospital. The study was approved by the Institutional Review Board of our institution (no. 2201–106–1291) on January 26, 2022; the requirement for informed consent was waived. The paper also adheres to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) criteria for observational studies [12].
EJV cannulation procedure
In our institution, EJV cannulation has been mainly performed for surgical patients with difficult large-bore IV access or those who need additional large-bore IV access during surgery (Fig. 1). Patients are placed in the Trendelenburg position, with the head slightly tilted to the opposite side of the EJV cannula insertion site. The pillow is removed to facilitate visualization of the EJV during the procedure. Due to the possibility of anatomical variation in EJV [13], ultrasound may be used at the discretion of attending anesthesiologist when the EJV is not readily visualized or palpable. After cleaning the insertion site with an alcohol swab, a needle is inserted at a shallow angle (approximately 10 degrees) above the EJV. When blood appears in the flash chamber of the catheter, the needle is advanced 1–2 mm farther. After that, the catheter over the needle is smoothly inserted while the needle is fixed, after which the needle is removed. After the catheter is successfully placed, it is connected to IV fluid bags. The success of catheter insertion is confirmed by successful blood aspiration via the catheter and no visible or palpable swelling after the administration fluid. EJV cannulation is routinely removed immediately after completion of surgery in the operating room or after the post-anesthesia care unit (PACU) or intensive care unit (ICU) admission. However, depending on the attending anesthesiologist, EJV access may be maintained after surgery for the administration of medication, fluids, or blood products. After removal of the EJV cannulation, manual pressure with a sterile gauze pad at the insertion site is applied by the attending anesthesiologists or nurses for at least 5 min.
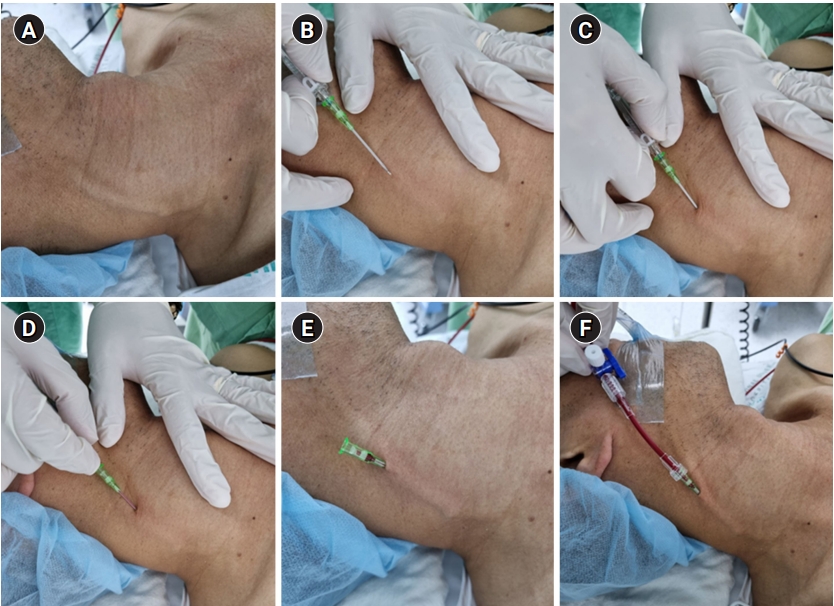
External jugular vein (EJV) catheterization. (A) Visualization of the EJV is facilitated. (B) The catheter is inserted over the needle at a shallow angle (approximately 10 degrees) above the EJV after cleaning the insertion site with an alcohol swab. (C) The needle is advanced 1–2 mm farther when blood appears in the flash chamber of the catheter. (D) The catheter is inserted over the needle smoothly while the needle is fixed. (E) The needle is removed. (F) The catheter is connected to fluid line and blood is aspirated via the catheter to confirm the success of catheter insertion.
Study population and data collection
This study included only adult (≥ 18 years) patients who underwent anesthesia for surgery and received EJV cannulation, performed by the attending anesthesiologists, in the operating room between 2010 and 2021. We collected data from 2010 as EJV cannulation data had been recorded in the electronic medical records (EMRs) since 2010.
In our institution, anesthesiologists routinely record the type (arterial-, peripheral-, or central line) and site of any vascular cannulation performed during anesthesia in the anesthetic records. To maximize the sensitivity for the screening of EJV cannulation cases during anesthesia, we used a search algorithm with the following keywords and their potential errata: “EJV”, “ext. jugular”, and “external jugular.” The anesthetic records were manually reviewed by two independent researchers to confirm the EJV cannulation.
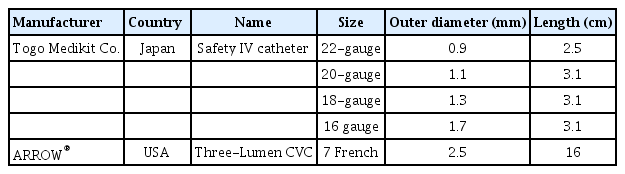
We reviewed the EMRs and recorded the following variables: age, sex, body mass index, surgery type, robotic surgery, laparoscopic surgery, emergency, discharged to intensive care unit, type of anesthesia (general, neuraxial, or monitored anesthesia care), and the amount of infused crystalloid, colloid, and blood products. The following EJV cannulation-related variables were also retrieved from the anesthetic records: insertion time (induction of anesthesia vs. during surgery), purpose (for fluid administration, central venous pressure monitoring, or both), insertion side (right, left, both, or not specified), insertion technique (blind technique vs. ultrasonographic guidance), type of catheter (16-, 18-, 20-, 22-gauge intravenous catheter, or central-line catheter), and connection to rapid infusion system. Information about the type and manufacturer of the catheter is provided in Table 1.
To evaluate the efficacy and safety of EJV cannulation, any EJV cannulation-related complications (insertion site swelling, infection, thrombophlebitis, pneumothorax, and arterial cannulation) were evaluated using the records identified for the present study. In addition, postoperative medical records, including progress notes, consultant notes, nursing records, and discharge notes, were also screened in the same manner to identify any EJV cannulation-related complications within 7 days after surgery. This information was then were manually reviewed by the researchers. Any disagreements between researchers were resolved through discussion. During the revision process, EJV cannulation-related death was investigated among the in-hospital death cases.
Statistical analysis
Descriptive statistical analyses was conducted using R software version 4.0.0 (R Core Team, 2020) (R: Language and Environment for Statistical Computing, R Foundation for Statistical Computing, Austria; https://www.r-project.org/). Continuous data are summarized as median (interquartile range) (range). The categorical variables are summarized as the number of patients (n) and proportions (%). Imputation for missing data was not performed.
RESULTS
We obtained the data of 9,577 (9,100 patients) from 494,447 anesthesia cases (339,077 patients) at our institution between 2010 and 2021 using a search algorithm for EJV cannulation during anesthesia. Patients who were found not to receive EJV cannulation during anesthesia after the review of anesthetic records (94 cases) and those who did not undergo surgery (1 case) were excluded from the analysis. Finally, a total of 9482 anesthesia cases of 9,062 patients were analyzed.
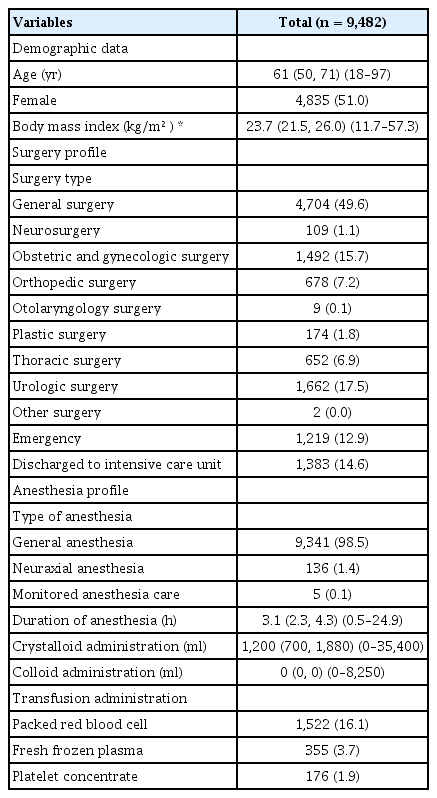
Table 2 includes the demographic data, surgery, and anesthesia-related profile information of patient cases considered in the study. For the analyzed cases, the most commonly performed surgery type was general surgery (49.6%), followed by urologic surgery (17.5%) and obstetric and/or gynecologic surgery (15.7%). Most patients received general anesthesia (9,341 cases, 98.5%), but some patients received neuraxial anesthesia (136 cases, 1.4 %) or monitored anesthesia care (5 cases, 0.1%).
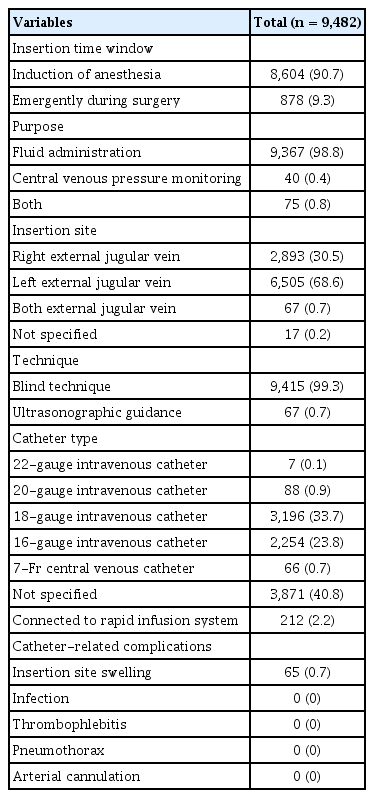
Table 3 presents the EJV cannulation-related data. In most cases, EJV cannulation was performed during anesthetic induction (9,604 patients, 90.7%); however, for 878 (9.3%) cases, unplanned EJV cannulation was performed emergently during surgery. The majority of emergent EJV cannulation were performed during general surgery (558 cases, 63.6%), followed by obstetric and/or gynecologic surgery (143 cases, 16.3%) and urologic surgery (83 cases, 9.5%). The main purpose of EJV cannulation was fluid administration (98.8%); in rare cases, EJV cannulation was performed solely for central venous pressure monitoring (0.4%). The most commonly performed cannulation technique was Lt. EJV cannulation (68.6%) under blind technique (99.3%) with an intravenous catheter size of 18-gauge or larger (58.2%). When the 7-Fr central venous catheter was used, the median duration of catheter placement was 1 day, and its range was 0–11 days. The EJV cannulation was connected to the rapid infusion system for 212 (2.3%) cases. The only EJV cannulation-related complication was swelling at the EJV-cannula insertion site (65 cases, 0.7%). Among them, 63 cases were recorded solely in the anesthetic record and resolved with manual compression during anesthesia without any requirement for further evaluation or treatment. Only two cases (0.02%), elaborated below, recorded in the postoperative medical records were determined to be related to EJV cannulation. Of the 160 in-hospital death cases included in the study, EJV cannulation-related death was not identified.
In the first of the two cases mentioned above, a 16-gauge IV catheter were placed at the right EJV during the anesthesia induction, and a total of 1,100 ml of crystalloid was infused over 145 min of anesthesia with an estimated surgical blood loss of 300 ml. During the PACU stay, a swelling on the right side of the patient's neck was found by a nurse before the removal of EJV catheter. The patient did not present with any related symptoms such as neck pain or dyspnea. The right EJV was then evaluated by a radiologist using ultrasound on the day after surgery, and no significant abnormalities were found. The patient was discharged without any other complications on postoperative day 4. In the second case, a 16-gauge IV catheter was placed at the left EJV during the anesthesia induction. The duration of anesthesia was 330 min, and the estimated surgical blood loss was 950 ml. A total of 2,750 ml of crystalloid and 500 ml of hydroxyethyl starch was infused through IV routes. After surgery, the adhesive surgical drape used to secure the catheter was removed, and edema from the left chest to the left cheek was observed. The cause of the edema was suspected to be the extravasation of fluid through the left EJV route, and the estimated amount of leakage was 700 ml. Concerned about the possibility of airway compression, the patient was transferred to the ICU under intubated status. The edema subsided on postoperative day 1. An endotracheal cuff-leak test was then performed to confirm the absence of post-extubation stridor, after which the patient was extubated. The patient was transferred to a general ward on the same day and discharged on postoperative day 8 without any complications.
DISCUSSION
This study investigated the feasibility and safety of EJV cannulation in surgical patients. During the 12 years of the study period, EJV cannulation was performed for 9,482 anesthesia cases from 9,062 patients, of which 878 (9.3%) cases were performed emergently during surgery. The only identified complication related to EJV cannulation in this study was swelling around the cannula insertion site, and no other complication was identified. Our results suggest the feasibility and safety of EJV cannulation for administering fluids in surgical patients.
EJV cannulation has been performed mainly for fluid administration in surgical patients in our institution. As a part of improving postoperative recovery, unnecessary CVCs have been gradually reduced to enhance early ambulation and recovery after surgery [14]. However, since unexpected intraoperative bleeding cannot be entirely avoided [15], the need for large-bore access IV remains for surgical patients.
Previous studies have debated the usefulness of EJV cannulation in surgical patients [1]. One randomized controlled trial (RCT) involving patients who underwent open-heart surgery reported that EJV cannulation required a longer procedure duration and had a higher failure rate than the antecubital venous cannulation [16]. Another RCT reported that the success rate of EJV cannulation was lower than that of ultrasound-guided peripheral IV cannulation for patients with difficult vascular access [1]. However, these two studies involved trainees inexperienced with EJV cannulation. We could not obtain information on the practitioners of EJV cannulation due to our retrospective study design; however, it is usually performed by an anesthesiologist experienced with EJV cannulation in our institution. Another RCT reported the low success rate of CVC via the EJV using the blind technique (10/30, 33%) and ultrasound-guided technique (6/30, 20%) [17]. However, this low success rate may have been due to their study participants (inexperienced trainees) and guidewire-guided CVC insertion. The anatomical variation in the EJV-SCV junction can contribute to the difficulty in inserting CVC via EJV [7]. We mainly used an IV catheter for EJV cannulation without using a guidewire, which could have contributed to the simpler implementation of EJV compared to CVC.
As EJV is directly connected to the central compartment, complications related to central venous catheterization, including bloodstream infection, arterial puncture, hematoma, pneumothorax, thrombosis, and air embolism, can theoretically occur after EJV cannulation [18]. However, in our study, no significant complications related to EJV cannulation were identified. Some previous studies reported that the only complication associated with EJV cannulation was a small subcutaneous hematoma at the failed insertion site, and there was no related arterial complication [19]. There have also been previous case reports of very rare but severe complications of EJV cannulation. One report was of a case of pulmonary air embolism through the open hub of an EJV cannula that was accidentally disconnected from the IV set in a patient who underwent bilateral humerus fracture surgery [20]. Another report was of a case of fracture and distal migration of the IV cannula placed in the EJV in the ICU patient [21]. Although we did not identify these complications in our patients, anesthesiologists should be careful of severe complications associated with EJV cannulation during cannula insertion, maintenance, and removal.
In our study, the only identified complication was swelling around the insertion site, which may have been due to extravasation caused by catheter tip malposition during surgery. There was only one case of an unplanned ICU admission due to swelling related to EJV cannulation. Since the extravasation of a large volume of fluids in the cervical area may cause airway obstruction [22,23], it may be helpful to assess the patency of the EJV cannula by inspection and palpation of the insertion site to minimize this complication. The unexpected extravasation of vasoactive drugs, hyperosmolar solution, and concentrated electrolyte solution may occur during anesthesia, which may lead to the necrosis of skin and subcutaneous tissue, even requiring surgery in rare cases [24]. In our study, skin necrosis was not identified during the review of medical records, probably because EJV access was mainly used for the administration of crystalloid or blood products in this study.
EJV cannulation was performed emergently during surgery for 9.3% of our cases, and most of them were for abdominal surgeries. These results may be attributed to the easier access to the EJV than peripheral veins at extremities during the abdominal surgery, as well as the ease with which EJV cannulation can be performed with blind techniques relative to internal jugular vein cannulation. Further, EJV cannulation may have a low risk of major complications due to anatomical characteristics. Therefore, EJV cannulation can provide safe and reliable IV access, especially when additional rescue IV access is emergently required during abdominal surgeries. However, anesthesiologists should pay attention to its high malposition rate due to the relatively common anatomical variation of EJV [25,26].
The results of our study should be interpreted with caution. First, this was a retrospective cohort study, and the complication rate may have been underestimated. We thoroughly screened the anesthetic and postoperative medical records using the search algorithm for any clinically significant complications. However, subclinical complications, such as mild insertion site swelling or extravasation, may have occurred without being documented in the medical records. Although the EJV catheters were removed immediately after surgery, unidentified EJV catheter-related bloodstream infections may have also occurred. In addition, only the amount of fluid or blood, or vasopressors administered through the entire IV routes, and not the EJV cannula, could be measured. Second, we could not investigate the success rate of EJV cannulation. EJVs in obese patients may be less visualized or palpable than those in non-obese patients. Further studies are warranted to examine the potential factors affecting the success rate of EJV cannulation, such as obesity and ultrasound guidance. Third, since most cases of EJV cannulation were performed by experienced anesthesiologists, the extent to which the results may be generalized to other institutions with less EJV cannulation experience is uncertain. Fourth, we did not include EJV cannulation cases in pediatric patients. Although there is evidence on the central venous access via EJV in pediatric patients [27,28], the feasibility of EJV cannulation with intravenous catheter in this population warrants further investigation. Lastly, we could not directly compare the feasibility and safety of EJV cannulation with that of other IV access.
In conclusion, our study showed the feasibility and safety of EJV cannulation for surgical patients. EJV cannulation was also useful for securing emergent IV access during surgery. No serious complications, except swelling around the insertion site, could be found in our study. EJV cannulation can be useful for safe and reliable IV access in surgical patients.
Notes
FUNDING
None.
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
DATA AVAILABILITY STATEMENT
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request and with permission of the Institutional Review Board of the Seoul National University Hospital.
AUTHOR CONTRIBUTIONS
Conceptualization: Ho-Jin Lee. Data curation: Jae-Woo Ju, Yoonbin Hwang. Formal analysis: Jae-Woo Ju, Yoonbin Hwang. Writing - original draft: Jae-Woo Ju. Writing - review & editing: Ho-Jin Lee. Supervision: Ho-Jin Lee.