Depth of double-lumen endobronchial tube: a comparison between real practice and clinical recommendations using height-based formulae
Article information
Abstract
Background
The depth of double-lumen endobronchial tube (DLT) is reportedly known to be directly proportional to height and several height-based recommendations have been suggested. This retrospective study was designed to find out the difference between calculated depths using height-based formulae and realistic depths in clinical practice of DLT placement by analyzing pooled data from patients intubated with left-sided DLT.
Methods
The electronic medical records of adults, intubated with DLT from February 2018 to December 2020, were reviewed. Data retrieved included age, sex, height, weight, and size and depth of DLT. The finally documented DLT depth (depth final, DF) was compared with the calculated depths, and the relationship between height and DF was also evaluated. A questionnaire on endobronchial intubation method was sent to anesthesiologists.
Results
A total of 503 out of 575 electronic records of consecutive patients were analyzed. Although the relationship between height and DF was shown to have significant correlation (Spearman’s rho = 0.63, P < 0.001), DF was shown to be significantly greater than calculated depths (P < 0.001). Despite 57.1% of anesthesiologists have knowledge of clinical recommendations to anticipate size and depth of DLT, no one routinely utilizes those recommendations.
Conclusions
Anesthesiologists tend to place DLTs in a deeper position than expected when depths are calculated using height-based recommendations. Although such discrepancies may not be clinically meaningful, efforts are needed to standardize the methods of endobronchial intubation to prevent potential complications associated with malposition.
INTRODUCTION
As video-assisted thoracoscopic surgery is preferentially employed for thoracic surgery, one-lung ventilation (OLV) is mandatory for surgical exposure [1]. Obviously, proper placement of the bronchial limb of the double-lumen endobronchial tube (DLT) is a vital part of the OLV procedure.
The depth of DLT, an important indicator for DLT placement, is reportedly known to be directly proportional to patient height [2,3] and several height-based formulae have been suggested in literature [2,4–8]. Although statistical significance was obtained, those formulae were shown to have a less than “moderate” correlation between height and depth of DLT (i.e., correlation coefficient < 0.6). Furthermore, those formulae were not clinically recommended in adults with short stature (< 155 cm) [9].
This retrospective study aimed to analyze data from patients whose tracheas were intubated with a left-sided DLT for operations requiring OLV. Additionally, the anesthesiologists whose practices were included into the analysis were asked to complete a simple questionnaire on how they perform the endobronchial intubation. The current investigation was designed to find out the difference between calculated depths using height-based formulae and realistic depths in clinical practice of DLT placement at two institutions.
METHODS
After receiving approval from the local ethics committees of participating hospitals to waive informed consent, the electronic medical records (EMR) of adult patients (≥ 20 years old), who required endobronchial intubation with DLT for OLV over a three-year period from February 2018 to December 2020, were reviewed. The exclusion criteria included no documentation of DLT depth and/or documentation of failure in maintaining OLV from desaturation, hypercarbia, or elevated peak airway pressure. When a patient had undergone more than two consecutive operations requiring OLV during the study period, only the more recent operation was included. The data retrieved included age, sex, height, weight, and size and depth of DLT. The current investigation was registered with the Clinical Research Information Service of the Republic of Korea (no. KCT 0005966).
The DLT intubation procedures were as follows. The size and anticipated depth of DLT was selected at the discretion of a board-certified anesthesiologist who oversaw the anesthesia care of a given patient. Anesthesia was administered using intravenous (IV) midazolam (1–3 mg), fentanyl (50–100 μg) and propofol (2 mg/kg) and muscle relaxation was provided with IV rocuronium (0.6 mg/kg). The trachea of the patient was intubated with a left-sided DLT, which was provided by two different manufacturers (Shiley™, Covidien, USA for 32, 35 and 37 Fr and Human-Broncho™, Insung Medical, Korea for 33 and 35 Fr). The methods used to confirm bronchial placement of the DLT were at the discretion of the assigned anesthesiologist, including auscultation and fiberoptic bronchoscope (FOB). The DLT was fixed at either corner of the mouth depending on the surgical requirement and its depth was measured at the upper incisor level using centimeter markings on the external surface of the DLT. The EMR template required the depth of DLT to be documented as follows. Initially, the depth of DLT was recorded at the discretion of the assigned anesthesiologist when it was finally considered to be adequate for OLV. In the middle of the study period, the requirement for documentation of DLT depth was changed to be two times; first, in the supine position and then in the decubitus position, designated as depth supine and depth decubitus, respectively. For comparison, the finally documented depth of the DLT, irrespective of the position in which it had been recorded, was designated as depth final (DF). If depths in both the supine and decubitus positions were available, the authors left the following remarks about the depth adjustment and adjustment distance as follows: no adjustment and zero (when both depths were the same), pull and negative distance (when DLT was withdrawn from the initially indwelt position), and push and positive distance (when DLT was advanced beyond the initial depth). The anticipated depth of DLT placement was calculated using height-based formulae suggested in previous studies [2,4–8]. The size of DLT was compared to the anticipated size based on sex and height [10]. The following qualifiers were used: match, smaller or bigger for same, smaller, or bigger size of DLT (size discrepancy). The patients included in the analysis were further categorized into four different height ranges, based on overall and sex-specific 25, 50, and 75 percentiles from Size Korea Database [11].
We surveyed the anesthesiologists whose practices were included in the current retrospective investigation about their methods to decide the size and depth of DLT. The first question was whether they had prior knowledge about recommendations to anticipate the size and depth of DLT based on the patient’s height and sex. The second was about how they chose the size of DLT, and then about how they decide the depth of DLT (Supplementary Table 1).
Categorical data are shown as number (percent) and continuous data are represented as mean ± SD or median (1Q, 3Q), as appropriate. Based on the normality test, parametric or non-parametric test was done appropriately. Correlation and simple linear regression were calculated to evaluate the relationship between height and DF, producing coefficients of correlation and determination (R2), respectively. A P value of < 0.05 was considered significant. Statistical analyses were performed with R studio (1.4.1103, R. RStudio, Inc., USA; http://www.rstudio.com/) and R version 4.0.3 (R foundation for Statistical Computing, Austria; https://www.R-project.org/).
RESULTS
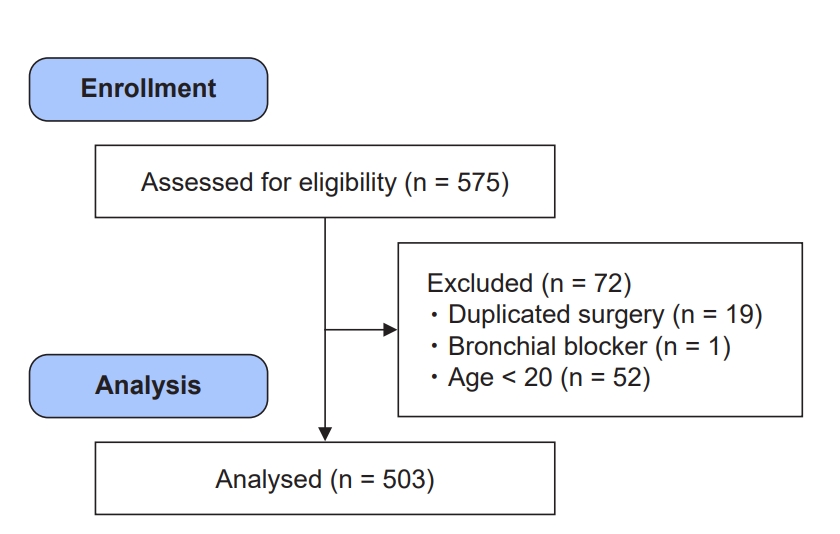
A total of 575 electronic records of consecutive patients whose tracheas were intubated with left-sided DLT for operations requiring OLV over the study period were reviewed. 52 records from patients who were less than 20 years old, 19 initial records of patients who had undergone duplicate operations over the study period and 1 record from a patient who had required bronchial blocker were excluded from analysis (Fig. 1). No failure in maintaining the OLV was documented.
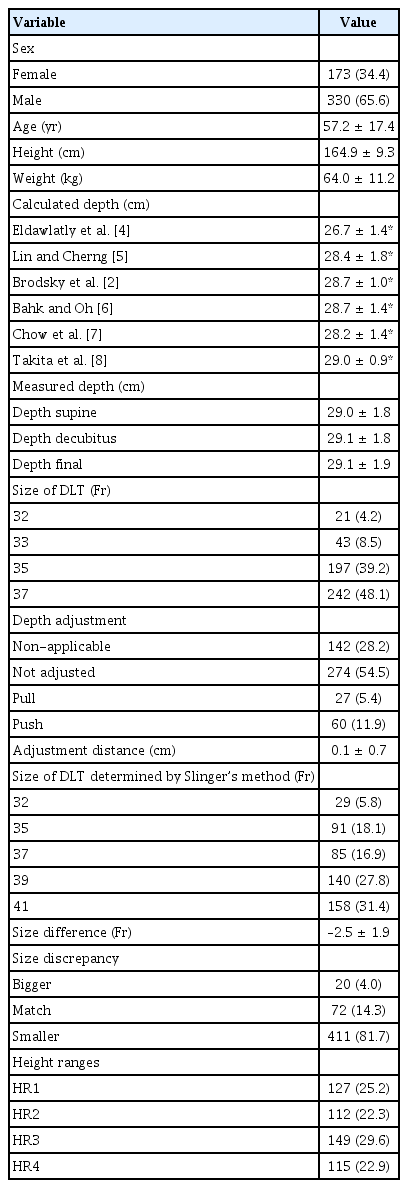
Table 1 represents the demographic and DLT-related data of the 503 patients. Compared to the calculated depths, the DF (29.1 ± 1.9 cm) was shown to be significantly greater (P < 0.001). Data on the adjustment of DLT depth after turning to the lateral position were available for 361 patients. The DLT was left in place in most patients (75.9%, 274/361). Although it was done in a relatively small number of patients, further advancement was more frequently done than withdrawal was (60 vs. 27, respectively). A DLT smaller than that anticipated using the Slinger method [10], was used in most patients (81.7%). Fig. 2 represents the relationship between height and DF for overall patients with significant correlation (Spearman’s rho = 0.63, P < 0.001) and the regression equation of DF = 8.36 + 0.13×Height (Adjusted R2 = 0.394, P < 0.001).
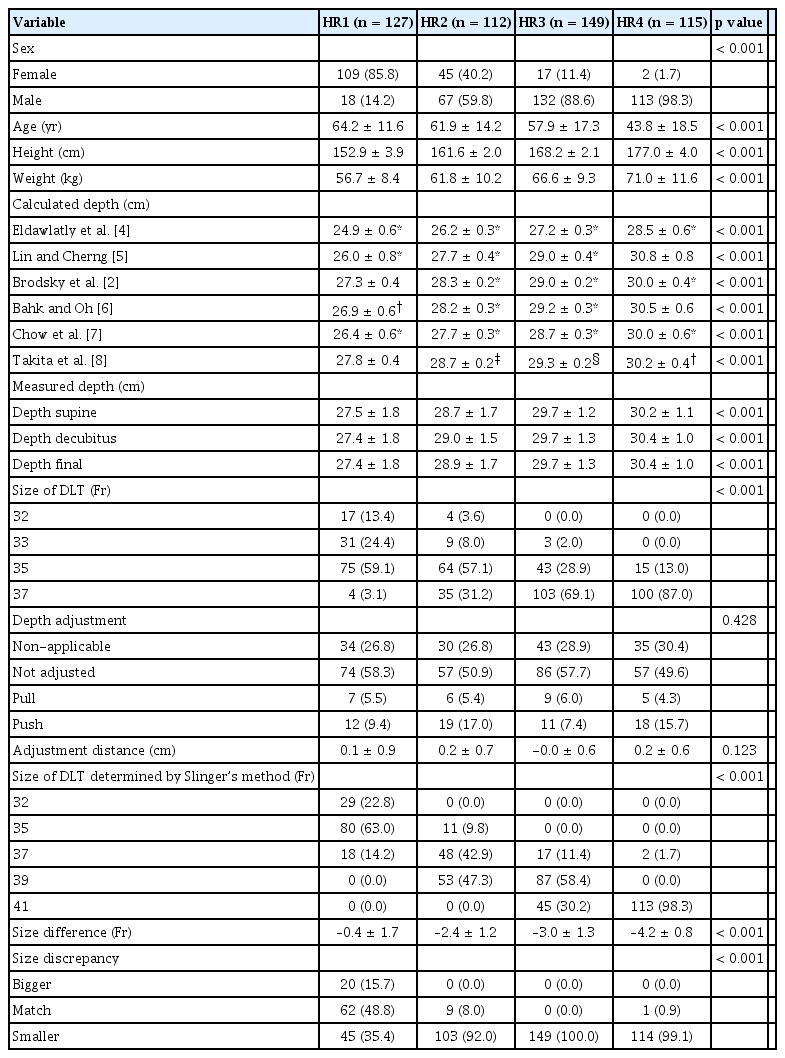
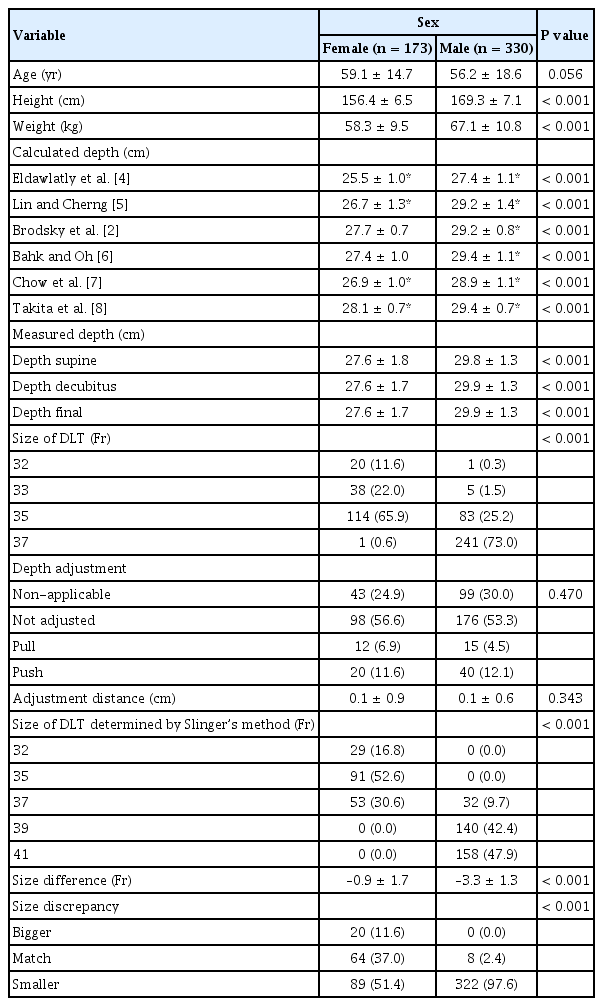
Tables 2 and 3 represent the demographic and DLT-related data, categorized by height range (HR; HR1, < 158 cm; HR2, ≥ 158 and < 165 cm; HR3, ≥ 165 and < 172 cm and HR4, ≥ 172 cm) and sex, respectively. The DF was shown to be significantly greater than the calculated depths (P < 0.05), except for those calculated by some formulae in HR1, HR4 and in female patients. Fig. 3A and 3B illustrates the relationship between height and DF in female and male patients, respectively, revealing a significant correlation between height and DF, in both female and male patients (P < 0.001).
A questionnaire about personal knowledge and methods of endobronchial intubation, consisting of four questions (Supplementary Table 1) was sent to 18 anesthesiologists, and 14 anesthesiologists of whom (77.8%) successfully completed it. Of the anesthesiologists, 57.1% (8/14) had knowledge of the recommendations to anticipate the size and depth of DLT based on height and/or sex. However, none reported routinely using those recommendations when performing endobronchial intubation. Most anesthesiologists (13/14, 93%) reported empirically choosing the DLT size based on a patient’s height and weight. Only one anesthesiologist reported referring to the diameter of the left bronchus retrieved from radiological evaluations. Regarding how to decide the depth of DLT, 57.1% (8/14) of anesthesiologists advance the DLT until moderate resistance is encountered, and then confirm the placement with FOB. Only 28.6% (4/14) of anesthesiologists place the DLT at the anticipated depth based on the literature. One anesthesiologist reported consistently deciding the depth of DLT using FOB, while another anesthesiologist adopted an arbitrary depth of DLT based on sex, which was subsequently confirmed using auscultation and FOB. The anesthesiologists preferentially (12/14, 85.7%) use auscultation to check the proper placement of the DLT, and subsequent FOB to confirm the placement. The remaining anesthesiologists prefer the FOB, and auscultation is only used to check bilateral symmetry. No one reported using only FOB to confirm the proper placement of DLT.
DISCUSSION
The current investigation on retrospectively pooled data from anesthetic practices with DLT for OLV demonstrated that the anesthesiologists working in the participating hospitals placed smaller DLTs at deeper levels than those anticipated using clinical recommendations based on height and sex. This tendency to place a smaller DLT at a deeper level was apparently demonstrated regardless of sex and height range.
A preoperative radiograph, such as a chest posteroanterior radiograph or chest computed tomography (CT), has been known to be little help to predict difficulty to be encountered during left endobronchial intubation [3,12]. It is commonly performed that a DLT is advanced until moderate resistance is encountered. As evidenced in the answers to the questionnaire in the current investigation, most anesthesiologists use such a “blind” method for initial placement of DLT. However, this method is known to easily produce DLT malposition, and even induce tracheobronchial damage, especially when a smaller-than-anticipated tube is used [13,14]. Therefore, a clinical guide to predict the depth of DLT prior to endobronchial intubation is required.
As the direction of DLT movement during lateral positioning or head rotation is almost always out of the bronchus [3,15], anesthesiologists tend to place the DLT as deep as possible to prevent dislodging. While most anesthesiologists agree that a bronchial cuff must be placed immediately below the carinal bifurcation, others suggest that the bronchial cuff must be advanced by 0.5–1.0 cm deeper into the bronchus because the DLT is easily moved proximally when the patient’s body or head is turned [16]. In a study on fiberoptic bronchoscopic measurements in Korean patients, the distance between the upper incisor and the upper margin of left mainstem bronchial carina was demonstrated to be 32.0 ± 2.1 cm in male, and 28.5 ± 2.0 cm in female [17]. The height of patients included in that FOB investigation (169.4 ± 6.1 cm in male, 158.4 ± 5.3 cm in female) was similar to that identified in the current investigation [17]. Therefore, the DF identified in the current investigation (29.1 ± 1.9 cm for overall patients, 27.6 ± 1.7 cm and 29.9 ± 1.3 cm for female and male patients, respectively) would not be considered too deep. Furthermore, recent investigations on the measurement of tracheobronchial tree in the Asian patients using chest CT demonstrated that the average length of left mainstem bronchus (tracheal bifurcation to the second carina) was 48.3 ± 6.5 mm [18]. The authors measured the length of the bronchial limb of the DLT used in the current investigation including bronchial balloon. It was 24–28 mm for Human-Broncho™ and 30–31 mm for Shiley™. Therefore, the left bronchial limb of the DLT has a safety margin of approximately 15–20 mm, which had been demonstrated in previous investigations on the measurement using FOB and CT scan in Korean patients [19, 20]. The differences between the average values of measured and calculated depths in the current investigation was < 20 mm. Therefore, statistically significant differences between the measured and calculated depths would not be “clinically” significant.
When the chest cavity is assumed to be a column, the sitting height is known for an important parameter to predict lung volume, estimating the height of the chest cavity [21]. The length of the tracheobronchial tree would be related to the sitting height. Asians have a relatively higher sitting height-to-leg length ratio, compared to the ratios in non-Asians [22], indicating that they have relatively longer torsos for a given height. Therefore, the previously suggested height-based formulae could underestimate the depth of DLT in Asians.
The depth of DLT would not be vital because the DLT depth is easily affected by postural changes of the head and neck. Furthermore, the optimal length of DLT is difficult to predict, along with intra-manufacturer variability in the dimensions of the bronchial cuff and tip, on which the margin of safety for insertion of the DLT depends [23]. However, DLT’s inserted too deep could predispose patients to tracheobronchial damage and potential barotrauma or pneumothorax [14]. Therefore, the anticipation of optimal depth matters to prevent the malposition of the DLT. Although FOB can help correct the position of the DLT, bronchoscopic misinterpretation of the carinal cascade can occur, especially in a patient with short stature; the second carina could be misidentified as the main carina, resulting in the obstruction of the left upper lobe. This may be attributed to the fear of DLT dislodgement by movement of the head and neck, wherein anesthesiologists tend to place a DLT at a relatively deeper position as the current investigation revealed. To prevent potential complications stemming from insertions that are too deep, the DLT position should be confirmed using FOB with standardized criteria. An institution’s own formula to predict the size or depth of the DLT based on its own patient characteristics would be suggested as a method of standardization, as demonstrated by Eldawlatly et al. [4,24].
The limitations of the current investigation are as follows. Although DF was measured after confirmation with FOB as an EMR template, unified criteria for FOB evaluation of DLT placement were not adopted. Thus, inter-practitioner variation might have occurred. Additionally, the DLT’s used in this investigation were from multiple manufacturers, which might have caused subtle differences in the detailed dimensions of the DLT, including the length of the bronchial limb and/or cuff, thus inter-manufacturer variation must be considered. Those inter-practitioner variations in FOB evaluation criteria and inter-manufacturer variations in DLT dimensions are, however, not considered clinically significant because all anesthesiologists uniformly confirmed the DLT placement using FOB with safety margin of approximately 20 mm in the bronchial limb of DLT irrespective of manufacturer. Although no documentation of failure in maintaining OLV was found, various record of non-fatal desaturation/hypoxia, hypercarbia or ventilatory difficulty could have been missed in the current retrospective investigation.
In conclusion, anesthesiologists working in the participating hospitals tend to place a smaller DLT at a deeper position, when compared to the size and depth calculated by clinical recommendations based on height. Such a discrepancy may not be clinically meaningful; however, efforts are needed to standardize the methods of endobronchial intubation to prevent potential complications associated with malposition.
SUPPLEMENTARY MATERIALS
Supplementary data including a questionnaire can be found online at https://doi.org/10.17085/apm.22214.
Questionnaire Distributed Among the Acting Anaesthetists
Notes
FUNDING
None.
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
DATA AVAILABILITY STATEMENT
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
AUTHOR CONTRIBUTIONS
Conceptualization: Jae Hee Woo, Jong Wha Lee. Data curation: Jae Hee Woo, Sooyoung Cho, Yongju Choi, Jong Wha Lee. Formal analysis: Sooyoung Cho, Jong Wha Lee. Methodology: Jae Hee Woo, Sooyoung Cho, Jong Wha Lee. Visualization: Sooyoung Cho. Writing - original draft: Jae Hee Woo, Sooyoung Cho, Youn Jin Kim, Dong Yeon Kim, Yongju Choi, Jong Wha Lee. Writing - review & editing: Jae Hee Woo, Sooyoung Cho, Youn Jin Kim, Dong Yeon Kim, Yongju Choi, Jong Wha Lee. Investigation: Yongju Choi. Resources: Youn Jin Kim. Software: Sooyoung Cho, Yongju Choi. Supervision: Youn Jin Kim, Dong Yeon Kim, Jong Wha Lee. Validation: Jae Hee Woo, Sooyoung Cho.