Management of unanticipated difficult airway in a patient with well-visualized vocal cords using video laryngoscopy - A case report -
Article information
Abstract
Background
Difficult airway occurs due to anatomical abnormalities of the airway that can be predicted through airway assessments; however, abnormalities beyond the vocal cord can be clinically asymptomatic and undetected until intubation failure to advance the endotracheal tube.
Case
We present a case of an unanticipated difficult airway in a stuporous 80-year-old female with a recent history of intracerebral hemorrhage and prolonged intubation. She required emergency ventriculo-peritoneal shunt surgery due to the progression of her hydrocephalus. Under anesthesia, facemask ventilation was easy and video laryngoscopy provided a full view of the glottis; however, endotracheal tube (ETT) entry failed. We suspected stenosis beyond the vocal cord, and a smaller diameter ETT was inserted and maintained for airway management during emergency surgery. Postoperative neck computed tomography findings revealed laryngotracheal stenosis (LTS).
Conclusions
Anesthesiologists should be aware that LTS may be asymptomatic and consider difficult airway guidelines in patients with history of prolonged endotracheal intubation.
Difficult airway is a challenging situation in which a trained anesthesiologist experiences difficulty or failure with one or more of the following: facemask ventilation, laryngoscopy, supraglottic airway ventilation, tracheal intubation, extubation, or invasive airway [1]. After easy facemask ventilation and full laryngoscopy visualization, it can be perplexing to experience difficulty with tracheal intubation when a challenge was not anticipated. Difficult intubation occurs due to anatomical airway abnormalities. Prediction of difficult intubation can be possible using physical characteristics such as obesity, restricted mandibular protrusion, higher Mallampati classification, short thyromental distance, and immobility of the neck [1,2]. However, anatomical abnormalities involving the larynx and trachea are frequently asymptomatic [3] and can remain unsuspected until difficult tracheal intubation during anesthesia. The narrowing anatomy of the upper airway that includes any part of the larynx and trachea is termed laryngotracheal stenosis (LTS). Major risk factors for LTS include previous tracheal intubation and prolonged duration; however, they are frequently overlooked during a pre-anesthetic evaluation because the patient may not exhibit symptoms suggestive of an airway abnormality [4].
We present a case of an unanticipated difficult airway in a stuporous 80-year-old patient with hydrocephalus who required emergency ventriculo-peritoneal (V-P) shunt surgery. After failing to advance an endotracheal tube (ETT) beyond the vocal cord despite a full view of the glottis using a video laryngoscope, we suspected anatomical narrowing of the larynx, and a smaller diameter ETT was inserted and maintained for airway management during surgery. Postoperatively, the patient remained intubated because difficult extubation was expected, and a neck computed tomography (CT) scan revealed LTS.
CASE REPORT
The publication of this case report was authorized by the Institutional Review Board (no. 2022-12-019), and the requirement for informed consent was waived.
An 80-year-old female (156 cm, 60 kg) with American Society of Anesthesiologists physical status classification IV required emergency V-P shunt surgery for her progressing hydrocephalus. She had been on medication for 12 years after being diagnosed with hypertension and cerebral infarction. Her most recent medical history includes admission to the emergency room four weeks ago for a stuporous level of consciousness. She was sedated due to agitated behavior and intubated in the emergency room with 7.5-mm inner diameter (ID) and 10.0-mm outer diameter (OD) plain cuffed ETT (Rüsch® Super Safety Clear™, Teleflex Medical) for ventilatory support. Brain CT indicated intracerebral hemorrhage in the left thalamus; subsequently, the patient underwent emergency surgery for stereotactic hematoma removal and external ventricular drainage. She remained stuporous and was mechanically ventilated in the neurosurgery intensive care unit (NSICU). On the third postoperative day, ETT cuff leakage was discovered, and the patient was re-intubated in the NSICU with another 7.5-mm ID and 10.0-mm OD plain cuffed ETT. Tracheostomy was scheduled for the tenth postoperative day, but it was not performed because the patient’s family members refused consent. The total duration of ETT placement was three weeks in the NSICU. After extubation, she was transferred to the general ward, and oxygen (2 L/min) was administered through a nasal cannula. Pulse oximetry readings were maintained from 97% to 99% without ventilatory support.
On the eighth day in the general ward, the neurosurgeon observed a dull response to external stimuli during routine rounding, and an external ventricular drainage obstruction was discovered. Brain CT indicated acute development of hydrocephalus, and the neurosurgeon requested emergency surgery for V-P shunt placement. A preoperative evaluation of emergency surgery was carried out. The patient did not exhibit any clinical signs of respiratory distress. Arterial blood gas analysis with oxygen (2 L/min) supply via the nasal cannula remained within the normal range (PaO2 114.9 mmHg, PaCO2 40.6 mmHg), and her chest x-ray was unremarkable (Fig. 1).
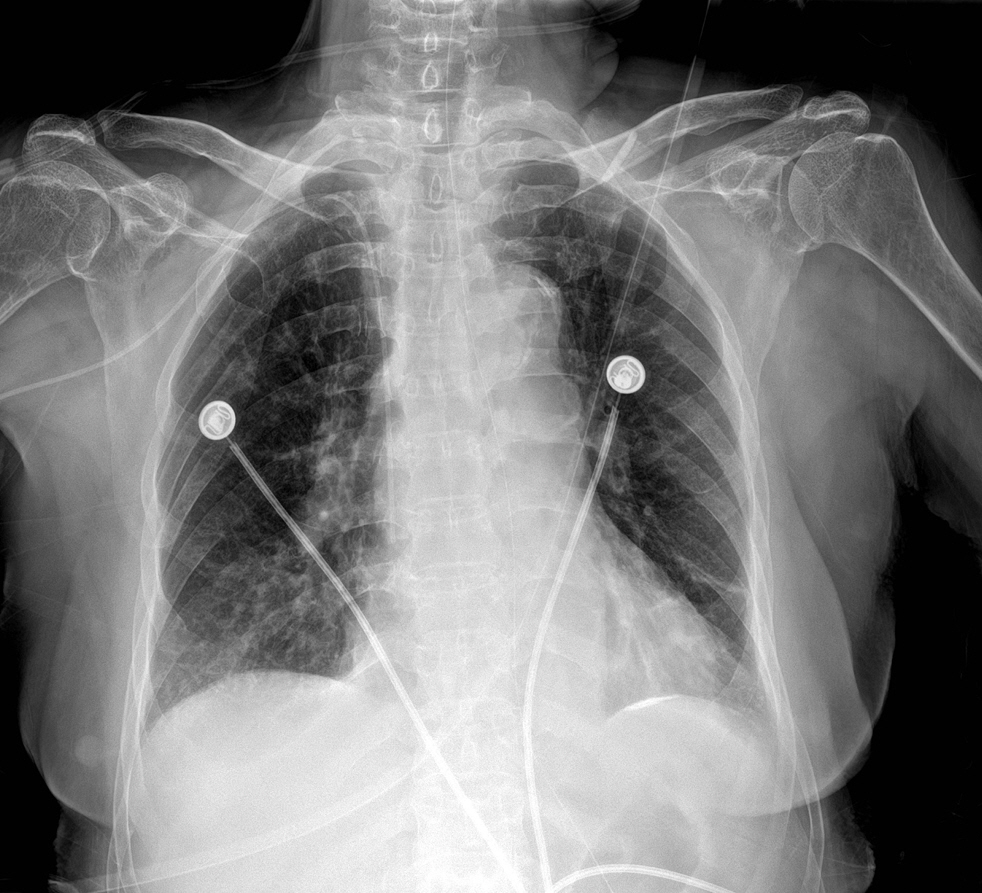
Supine anteroposterior chest x-ray was taken on the day of emergency ventriculo-peritoneal shunt surgery. There are no suspicious signs of tracheal abnormality.
In the operating room, the patient was uncooperative, but had regular spontaneous breathing with no signs of excessive effort, wheezing, or stridor. The patient was monitored with electrocardiograph electrodes, noninvasive blood pressure, pulse oximeter, and electromyograph TwitchView® (Blink Device Co.). The oximetry reading was 98% in room air. After 3 minutes of preoxygenation, we administered propofol at 1.5 mg/kg, rocuronium at 0.6 mg/kg, and remifentanil at 0.05 μg/kg/min through continuous infusion. Facemask ventilation was performed for 3 minutes without excessive resistance.
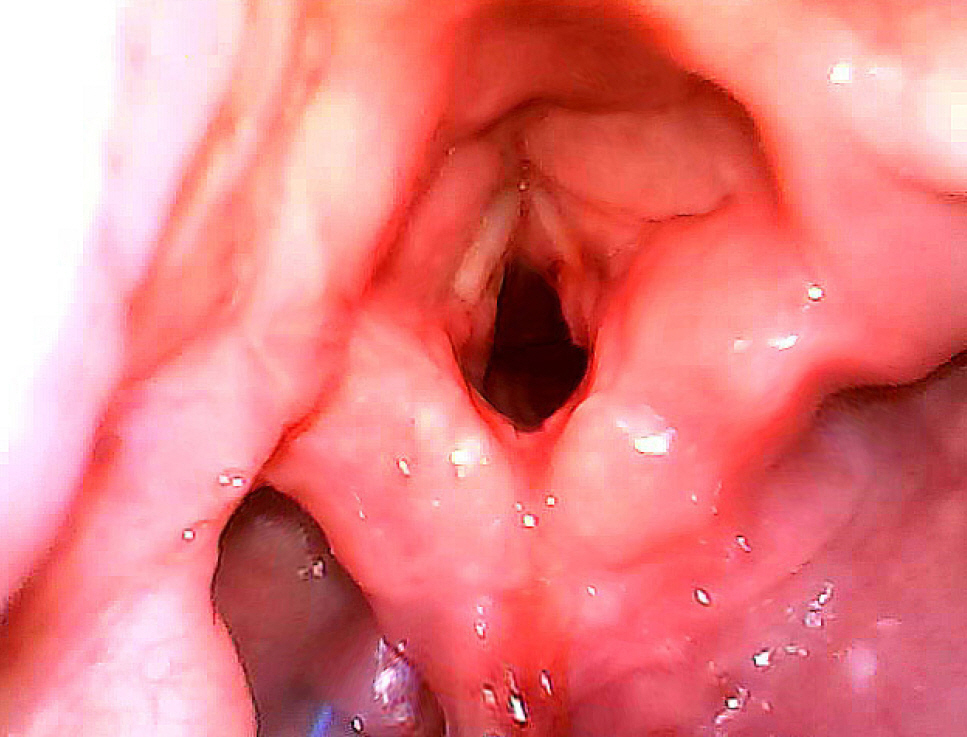
Intubation was initiated after the train-of-four count confirmed deep neuromuscular block. Video laryngoscope Insighters® (iS3, Shenzen Insighters Medical Technology Co.) was used for intubation as part of the department’s routine for safe intubation in the operating room. The video laryngoscopy provided us with a full view of the glottis (Fig. 2). The posterior one-half of the true vocal cord was not fully visible due to posterior glottic edema. There was no visible narrowing or stenosis of the subglottic space. Initial intubation was attempted with 7.0-mm ID and 9.7-mm OD ShielyTM Lo-Contour flexible reinforced cuffed ETT (Covidien Ireland Limited). However, the tip of the tube failed to advance 2 cm beyond the vocal cord. A second attempt was made immediately using 6.5-mm ID and 8.8-mm OD ShielyTM Lo-Contour flexible reinforced cuffed ETT, which also failed entry in the same way. Video laryngoscope was removed, and facemask ventilation was resumed.
Facemask ventilation was without excessive pressure and the oximetry reading remained at 100%.
We informed the neurosurgeon of the suspected narrowing beyond the glottis and recommended comprehensive airway evaluation, including consultation with an otolaryngologist. However, the neurosurgeon stated that emergency surgery could not be delayed due to the severity of hydrocephalus and requested for an additional intubation attempt using a smaller diameter ETT. An emergency airway cannulation was prepared in the event of airway obstruction, and a third intubation attempt was made using a 5.5-mm ID and 7.5-mm OD ShielyTM Lo-Contour flexible reinforced cuffed ETT. The tube advanced with resistance beyond the vocal cord, and ventilation was confirmed using capnography. The tracheal tube cuff was gently inflated using a pressure cuff gauge (MallinckrodtTM Hand Pressure Gauge, Covidien Deutschland GmbH) until the pressure reached 20 cmH2O. Ventilation was performed without excessive airway pressure, with a peak inspiratory pressure between 25 and 30 cmH2O. We administered 5 mg of dexamethasone to reduce airway edema that may have been caused by multiple intubation attempts. The surgery was completed as planned, and the patient remained intubated and transported to the NSICU under manual ventilation with an oxygen supply of 8 L/min. Postoperative neck CT findings confirmed LTS involving the bottom part of the larynx (subglottis) and the cervical portion of the trachea (Fig. 3). Enlargement of both thyroid glands with multiple nodules was incidentally found. Otolaryngologist was consulted, and family members gave consent to surgical tracheostomy which was performed on the fifth postoperative day after V-P shunt surgery. The patient remained bedridden in a stuporous mental state with ventilation support for an additional 6 days before being transferred to another hospital. There were no other respiratory complications.

Axial (A), coronal (B), and midline sagittal section (C) of computerized tomography of the neck with 5.5 mm internal diameter cuffed reinforced endotracheal tube in place. Focal stenosis (white triangle) of the upper airway involves the subglottis and cervical part of the trachea. Enlargements of both thyroid glands with multiple nodules do not affect the cartilage structure of trachea.
DISCUSSION
LTS comprises a broad set of diagnoses characterized by narrowing anatomy of the upper airway, including the glottis, supraglottis, subglottis, and trachea, and is associated with severe and potentially fatal respiratory compromise [3]. LTS is most commonly acquired from prolonged intubations in which the endotracheal cuff pressure exceeds the tracheal mucosa's mean capillary pressure (> 30 mmHg) [3,5]. Excessive pressure leads to ischemia, granulation tissue formation, and scarring within the lumen strictures [4,5]. The most common symptoms of LTS from any etiology are hoarseness, wheezing, stridor, and nonproductive cough [3-5]. However, because the majority of patients are asymptomatic until the trachea is reduced to at least more than half of its original diameter, medical history and physical examination may not predict difficult airways [5].
We did not suspect anatomical narrowing below the glottis until after the intubation entry failure. During our emergency pre-anesthetic evaluation, the patient displayed no signs of respiratory distress, such as stridor or wheezing, and we were unable to assess for throat pain, hoarseness, or dysphonia due to the patient’s stupor. Preoperative arterial blood gas analysis was normal, and a chest x-ray prior to surgery revealed no evidence of tracheal abnormality (Fig. 1). The patient did not exhibit abnormal anatomical characteristics of difficult intubation predictors such as obesity, mandibular protrusion, high Mallampati classification, short thyromental distance, and immobility of the neck. Furthermore, we were given an initial impression of easy airway management because of the patient’s recent history of two successful intubations by non-anesthesiologists.
Traumatic tracheal intubation is a major factor in the development of LTS. Larger and less flexible ETT, excessive cuff pressure (> 30 mmHg), and poor intubating conditions such as insufficient sedation or muscle relaxation are major factors of tracheal injury. A larger ETT can impinge on laryngeal structures, causing vocal cord damage, and contact the subglottic mucosa, causing lacerations, erosions, or tracheal rupture [5,6]. Larger tubes have a longer cuff, which will lie more proximally in the trachea closer to the vocal cords and be associated with a longer segment of mucosal tracheal compression [6]. Furthermore, prolonged endotracheal intubation is strongly associated to the development of LTS, which can also result in tracheomalacia, tracheoesophageal fistula, granuloma, or other tracheal structural changes [7]. Therefore, patients who require prolonged intubation, defined as more than 7 to 14 days of intubation, should consider tracheostomy [7,8]. The proper ETT size for our patient, a female with a height of 156 cm, should have been 7.0-mm ID or smaller. Prior intubations using 7.5-mm ID plain cuff ETT by other departments may have been attributed to tracheal injury in addition to three weeks of prolonged intubation in NSICU.
The 2022 American Society of Anesthesiologists Practice Guideline for Management of the Difficult Airway defines difficult intubation as tracheal intubation that necessitates multiple attempts. Failed intubation attempts after general anesthesia induction necessitates a non-emergency pathway when mask ventilation is adequate, which includes considering awakening the patient or using alternative intubation approaches [1]. After our intubation entry failure, awakening the patient under mask ventilation would have been the safest approach because anatomical narrowing was suspected. Comprehensive airway evaluation with an otolaryngologist consultation can identify the cause of failed entry and enable us to plan for airway management, such as tracheostomy before surgery. However, in our case, the emergency surgery could not be postponed, and successful airway management was critical.
Alternative intubation techniques such as the use of a supraglottic airway device or laryngeal mask airway (LMA) can be used for difficult intubation when mask ventilation is possible [1]. According to Parmet et al. [9], LMA has a 94% success rate in providing rescue ventilation in difficult airway management. Agarwal and Shobhana [10] advocate the use of LMA in patients undergoing short neurosurgeries. However, in the case of our patient who required V-P shunt surgery, LMA was not ideal because manipulation in the neck occurs while tunneling the ventricular catheter to the peritoneum, and because the head is not fixed, the LMA can be displaced during surgery [11]. Therefore, we decided to retry tracheal intubation with a small tube after preparing the tracheostomy so that it could be performed immediately in an emergency. However, repeated intubation attempts should be approached with caution because they can cause further structural injury and obstruction, eventually leading to respiratory compromise and arrest [12,13]. The Difficult Airway Society (DAS) guidelines recommend limiting intubation attempts to 3 + 1 [12]. Because we had used video laryngoscopy since the first intubation attempt, we considered the third to be the final intubation attempt. Fortunately, the third intubation attempt was successful.
During our third intubation attempt, a 5.5-mm ID reinforced cuffed ETT advanced beyond the vocal cord with resistance, indicating anatomical narrowing of the subglottis and possibly trachea injury. Intubation with a small tracheal tube raises concerns about the safety and conduct of anesthesia. Small-diameter ETT has a smaller luminal cross-sectional area and higher resistance to airflow, resulting in higher peak inspiratory pressure during positive ventilation and increased resistance to expiratory airflow [6,8]. Small ETT may easily become obstructed from the patient’s viscous secretions that require suction with an elevated risk of lung collapse and hemodynamic instability when the ratio between other diameters of the suction catheter and the ID of the tracheal tube surpasses 50%, as well as the risk of aspiration and air-leak under positive pressure ventilation due to inability to seal the trachea [6]. Our patient experienced none of the aforementioned issues during surgery.
We followed the DAS guidelines for the management of tracheal extubation, which define “at-risk” extubation as when risk stratification indicates that the patient may be unable to maintain his/her own airway after extubation or reintubation may be difficult [14]. We decided to postpone extubation because our patient met both factors of “at-risk” extubation; thus, the patient required a comprehensive airway assessment, such as a neck CT and otolaryngologist consultation, in a non-emergency setting. Fortunately, no additional damage, such as bleeding, was found in the postoperative neck CT results. However, if fiberoptic bronchoscopy-assisted intubation had been conducted as described by Hasegawa et al. [15], it would have been possible to confirm tracheal stenosis as well as perform atraumatic intubation in situations where surgery could not be postponed.
This case describes our experience of a stuporous patient with undiagnosed LTS whose vocal cords were visible using video laryngoscopy but whose airway management was difficult due to ETT entry failure. In similar situations, we recommend following guidelines for difficult airway management, as well as following extubation guidelines to reassess the risk of extubation. Anesthesiologists should be aware that LTS may be asymptomatic and perform comprehensive airway evaluations with fiberoptic bronchoscopy and imaging studies in addition to multidisciplinary approach in patients with risk factors for LTS, such as a history of prolonged endotracheal intubation. Lastly, prevention of LTS should be conducted in the routine practice of airway management by understanding the characteristics of ETT and avoiding traumatic intubations.
Notes
FUNDING
None.
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
DATA AVAILABILITY STATEMENT
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
AUTHOR CONTRIBUTIONS
Writing - original draft: Seunghee Ki, Seung Bae Cho. Writing - review & editing: Seunghee Ki, Seung Bae Cho, Jeonghan Lee. Investigation: Seunghee Ki, Seung Bae Cho, Seongmin Park, Jeonghan Lee. Supervision: Jeonghan Lee.