|
 |
- Search
| Anesth Pain Med > Volume 18(3); 2023 > Article |
|
Abstract
Background
COVID-19 and delayed hip surgery are well-known risk factors for thromboembolism in elderly patients.
Case
We report the case of an 88-year-old female patient with COVID-19 and pulmonary thromboembolism (PTE) who underwent delayed hip surgery 21 days after the injury. Heparinization and inferior vena cava filters were used to treat and prevent PTE. Transesophageal echocardiography and extracorporeal membrane oxygenation sheaths were inserted as a precaution in case of emergencies during surgery; the procedure was performed without any specific event.
With the increase in elderly population, the rate of hip surgeries in elderly patients is gradually increasing. Worldwide, more than 1.5 million adults are diagnosed with hip fractures annually [1]. Early hip surgery is known to be effective in reducing mortality, and surgical treatment is recommended as soon as possible after injury [1]. Delayed surgery for hip fractures is a well-known risk factor for venous thromboembolism [2]. The overall incidence of thromboembolic disease in patients with hip fracture is 11.9%. Delayed surgery increases the incidence and relative risk of thromboembolic disease. When surgery was delayed by one day, the incidence and relative risk increased to 14.5% and 2.32, respectively, while after seven days, the incidence was 33.3% and the relative risk was 3.71 [2]. Therefore, hip surgery is recommended at the earliest following injury. However, the recent coronavirus disease (COVID-19) era has led to some delay in surgeries due to screening and quarantine [3]. Several studies have reported that COVID-19 can induce a hypercoagulable state and cause multiple thromboembolic events [4].
We report a case of intraoperative anesthetic management in a patient with preoperative asymptomatic pulmonary thromboembolism (PTE) who tested positive for COVID-19 after a hip fracture and and underwent delayed surgery 21 days after injury. ŌĆā
Written informed consent for the procedure and publication of this report was obtained from the patient and her family members. The Institutional Review Board waived the review of this case (IRB no. 2022-12-015). This case report was written according to the recommendations of the Case Report (CARE) guidelines.
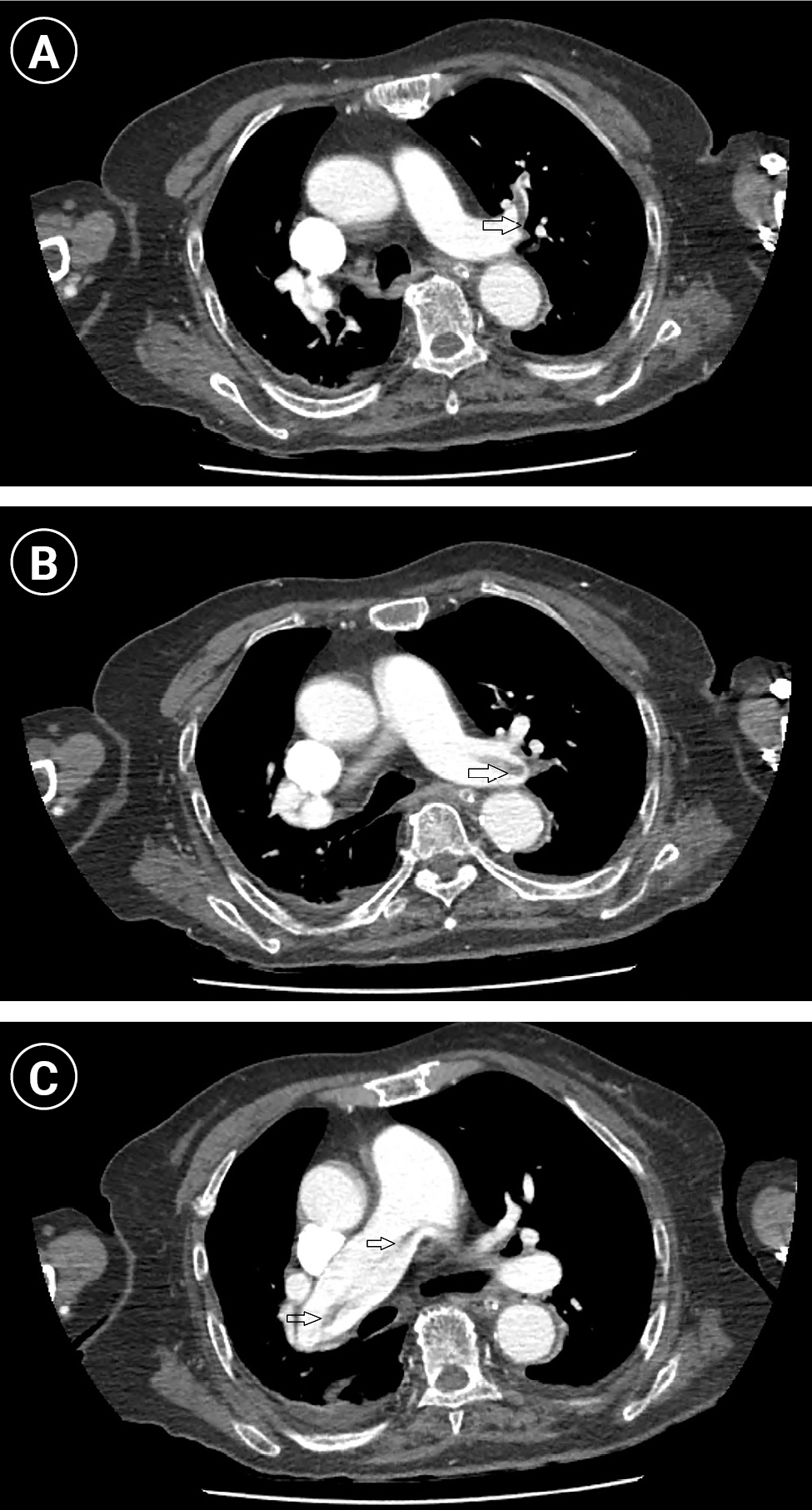
An 88-year-old female patient (height, 150 cm; weight, 50 kg; body mass index, 22.2 kg/m2) was transferred to our hospital with right hip pain after falling while walking using a walker 18 days before the hospital visit. The patient had a history of hypertension and dementia. After several days of conservative observation at home, there was no improvement in the hip pain. Initially, she visited another hospital four days after the injury, was diagnosed with an intertrochanteric fracture, and underwent the planned surgical treatment. During the preoperative evaluation, the patient was diagnosed with COVID-19 and transferred to an isolation ward. After one day in the isolation ward, the patientŌĆÖs blood pressure (BP) dropped to 94/39 mmHg due to urinary tract infection, sepsis, and ischemic colitis, and she was transferred to the intensive care unit (ICU). Therefore, the patient could not undergo the planned surgery. After treatment for ischemic colitis and septic shock, the patient was transferred to our hospital for surgical treatment 18 days after the injury. Preoperative laboratory findings were as follows: hemoglobin, 9.0 g/dl; platelet, 169,000 ┬Ąl; serum albumin, 3.28 g/dl (normal range 3.5-5.2 g/dl); C-reactive protein, 2.7 mg/dl; sodium, 139 mEq/L (normal range 136-145 mEq/L); arterial blood gas analysis, pH 7.55, pCO2 37 mmHg, PO2 63 mmHg, HCO3- 32.1 mmol/L, SaO2, 94.1%; prothrombin time (PT), 14.8 s; international normalized ratio, 1.21; activated partial thromboplastin Time, 35.3 s; and D-dimer of 18.94 ┬Ąg/ml (normal range < 0.5 ┬Ąg/ ml). To evaluate COVID-19 pneumonia, we performed chest computed tomography (CT), which showed diffuse PTE in both the main and left upper lobe lobar/segmental pulmonary arteries, consolidation in the right lower lobe, ground glass opacity in both lower lobes, a small amount of right pleural effusion, and left 4-9th, 11-12th rib fractures (Fig. 1A, B, C). Abdominopelvic CT scan revealed deep vein thrombus (DVT) in the left common iliac vein and left external iliac vein. Transthoracic echocardiography revealed a 65% ejection fraction, mild aortic stenosis, a thickened and calcified mitral valve with trivial mitral regurgitation, and visible echogenic material in the left atrium; however, electrocardiography showed no atrial fibrillation. Cardiology consultation recommended delayed surgery 2-3 days after heparinization as prophylaxis for the ongoing PTE and insertion of an inferior vena cava (IVC) filter (ALN Optional Vena Cava Filter with Hook, ALN) (Fig. 2). The patient was admitted to the operating room for planned right hip hemiarthroplasty. Preoperative vital signs were BP 165/78 mmHg, heart rate 72 beats/min, body temperature 36.5Ōäā, respiratory rate 20/min, and oxygen saturation 91% with two liters of O2 through nasal prongs. During surgery, the continuous radial arterial pressure, train-of-four (TOF), and bispectral index (BIS) were monitored. Anesthesia was induced using remimazolam (5 mg/kg/h) and rocuronium (35 mg). After confirming a BIS of 40 and 0% TOF, tracheal intubation was performed. Anesthesia was maintained using remimazolam (1 mg/kg/h) and remifentanil (0.2 ┬Ąg/kg/min). We chose remimazolam as the induction and maintenance agent to reduce hemodynamic instability. The cardiac surgery team judged it challenging to cannulate the patient and initiate extracorporeal membrane oxygenation (ECMO) immediately in case of a sudden cardiac arrest as the surgery was performed in the left lateral decubitus position. Therefore, the cardiac surgery team inserted an introducer sheath (Prelude┬« sheath introducers 5 Fr, Merit medical systems, Inc.) into the right femoral artery and vein, for performing ECMO, to be connected in case of an emergency. For intraoperative transesophageal echocardiography (TEE) monitoring, a TEE probe was inserted to evaluate the thrombus in the left atrium; however, no thrombus was observed. The patientŌĆÖs mean arterial pressure was maintained at over 70 mmHg during surgery by administering an ephedrine bolus of 5 mg four times. The total amount of fluid administered to the patient was 1,400 ml of plasmalyte, the amount of bleeding was 300 ml, and the urine output was 90 ml. The total anesthetic time was 190 min and the total operating time was 170 min. At the end of the surgery, all anesthetics were stopped, and 0.2 mg of flumazenil was used to reverse remimazolam. The patient had a TOF of 100% and was administered pyridostigmine (10 mg) and glycopyrrolate (0.2 mg) to reverse muscle relaxation. The patient was able to breathe spontaneously and tracheal extubation was performed without any complications. The patient was transferred to the ICU. On postoperative day 2, the ECMO sheaths were removed, and the patient was transferred to the general ward without any specific events. The IVC filter was removed on postoperative day 8, and the patient was discharged without any complication.ŌĆā
The patient was diagnosed with COVID-19 and asymptomatic PTE, and was administered general anesthesia after inserting an IVC filter before surgery. The patient scored 88 points on the pulmonary embolism severity index (PESI), which is used as a risk stratification tool for PTE. The patientŌĆÖs PESI was solely influenced by her advanced age of 88 years and not by the other ten clinical criteria used to calculate PESI score such as sex, history of cancer, respiratory rate, temperature, or history of heart failure. However, this score represents a moderate-risk group with an expected 30-day mortality rate of 3.2-7.1%, and higher levels of care are recommended [5]. Hip fracture surgery is recognized as a surgical procedure with a heightened risk of venous thromboembolism. Several factors, including advanced age, female sex, elevated body mass index, and surgical procedures lasting over two hours, have been identified as potential risk factors [6]. Delayed surgery in patients with hip fractures is also a risk factor for thromboembolism [2]. To reduce delirium and postoperative hospital stay, accelerated surgery, that is, surgery within 6 h after injury, has been proposed [1]. Therefore, even during the COVID-19 era, early surgery is advantageous for favorable patient outcomes. However, in this case, the patient stayed home for four days after the injury, and the operation was postponed because of sepsis.
Several studies have reported that COVID-19 infection itself is associated with PTE. According to a meta-analysis, the incidence of PTE in patients with COVID-19 is 14.7% in the general ward and 23.4% in the ICU [7]. This result represents a higher incidence compared to 2.1% in ICU patients during the pre-pandemic period [8]. In addition, the incidence of PTE in COVID-19-infected patients was nine times higher than that in non-COVID-19 patients. The in-hospital mortality of COVID-19-infected patients with PTE was 16.6%, similar to 16.0% in COVID-19 patients without PTE; therefore, it seems that PTE does not make a big difference in COVID-19 mortality. However, compared with the in-hospital mortality of 6.5% in non-COVID-19 patients with PTE, the mortality rate of COVID-19 patients with PTE is more than twice as high [9].
The exact epidemiology and pathophysiological mechanisms related to COVID-19-associated PTE remain unknown. Several studies have reported that COVID-19 increases the probability of thromboembolism [4,10]. Several factors are associated with the mechanisms related to the hypercoagulable state in COVID-19 patients [4]. First, direct and indirect factors such as severe hypoxia, underlying diseases, and organ dysfunction caused by COVID-19 may be associated with various hemostatic abnormalities [10]. Second, complement activation and cytokine release may result in proinflammatory and procoagulant effects due to endothelial dysfunction, von Willebrand factor elevation, Toll-like receptor activation, and tissue-factor pathway activation. Dysregulation of the coagulation cascade leads to the formation of intraalveolar systemic fibrin clots [4]. Third, releasing proinflammatory cytokines called ŌĆśCytokine stormŌĆÖ increases the risk of intravascular microthrombosis and induces secondary local consumption coagulopathy [10]. Fourth, the interactions between several blood cell types may be a critical factor in the pro-coagulant effect of viral infections [4]. Due to the hypercoagulable state, patients with COVID-19 present with higher levels of D-dimer, fibrinogen and fibrinogen degradation products, prolonged prothrombin time, international normalized ratio, and thrombin time [4]. These coagulation abnormalities are associated with a poor prognosis [8]. The patient, in this case, also showed an increase in D-dimer to 18.94 ┬Ąg/ml, which indicated the presence of PTE.
Since the COVID-19 pandemic, there have been concerns regarding delays in transporting trauma patients to hospitals due to the collapse of the healthcare system. According to Jarvis et al. [11], after the COVID-19 pandemic, the time to visit the hospital after the injury (injury to hospital arrival time) required for patients undergoing hip surgery took an average of 11.5 min longer than that before the pandemic. Nevertheless, this was not clinically meaningful, and there was a significant difference in the injury-to-hospital arrival time only when the number of infections surged during the early stages of the pandemic. However, the in-hospital mortality rate was 3.4% after the pandemic compared to 1.1% before the pandemic. According to Kim et al. [3], there was no significant difference in the overall time to surgery before and after the pandemic; however, the proportion of cases in which surgery was delayed by more than 36 h increased significantly after the pandemic. The reason for the delay in surgery was the time needed for medical investigation and stabilization. Preoperative tests and examinations that should be performed outside the isolation room or in contact with other people, such as electrocardiography, pulmonary function tests, and imaging, were postponed, and the patient was quarantined until the COVID-19 test was negative. In this report, 30-day mortality did not differ before and after the COVID-19 pandemic. According to a meta-analysis comparing the prognosis of patients who underwent hip surgery before and after COVID-19, there was no significant difference in the 30-day mortality [12]. However, a comparison between COVID-19-infected and non-infected patients revealed higher mortality rates in the former [12]. It is difficult to generalize the situation because of regional differences between the COVID-19 epidemic period and the medical system. However, except for some surges in COVID-19 infections, early hip surgery was performed similarly to that in the pre-pandemic period. Postoperative mortality was similar but increased in COVID-19-infected patients.
In patients who underwent total hip/knee arthroplasty in April 2020, when the lockdown was implemented due to COVID-19 in the United States, the incidence of PTE/DVT after surgery increased more than three-fold compared to the same period before the pandemic [13]. The authors suggested that the reasons for immobility were a decrease in activity during the initial lockdown of the pandemic and COVID-19. Although patient history of COVID-19 was not investigated, the authors noted that asymptomatic COVID-19 infection may have increased the incidence of PTE/DVT in unknown patients. Cuthbert et al. [14] reported that postoperative ICU admission was 27% in COVID-19-positive patients with hip fractures after the pandemic compared to 5% in COVID-19-negative patients. In addition, the length of hospital stay (median 23 days vs. 9 days, P < 0.001) and 30-day mortality (29% vs. 10%, P = 0.001) increased, and thromboembolic events occurred in 9.8% of COVID-19 positive patients.
An IVC filter was inserted to prevent additional thromboembolic events before surgery. IVC filters are recommended when a patient has venous thromboembolic disease, with an absolute contraindication to anticoagulation, problems that require stopping anticoagulation, or recurrent venous thromboembolism after receiving appropriate anticoagulation [6]. Because surgery was planned for our patient, anticoagulation therapy could not be continued for a sufficient period. Therefore, an IVC filter was inserted. In our patient, an ECMO sheath was inserted in advance, along with an IVC filter, to prepare for cardiac arrest. Although there are no specific guidelines for ECMO preparation in stable patients, ECMO was necessary because of the patientŌĆÖs advanced age and the lateral position required for surgery. Delaying ECMO initiation by more than 30 min in cases of acute pulmonary embolism can result in worse patient outcomes. [15].
In conclusion, this case report presents a geriatric patient diagnosed with a hip fracture, COVID-19, and asymptomatic PTE. Despite sepsis-related delays in hip surgery, general anesthesia was safely administered after heparinization and insertion of an IVC filter. Given the inevitability of delayed hip surgery in patients with COVID-19, the likelihood of developing PTE is significantly increased. Hence, the evaluation and prophylaxis for this condition are of utmost importance.
Notes
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
AUTHOR CONTRIBUTIONS
Conceptualization: Min Hee Heo, Ji Yeon Kim, Won Joo Choe, Jun Hyun Kim. Data curation: Sang Il Lee, Kyung-Tae Kim. Formal analysis: Jang Su Park. Visualization: Min Hee Heo, Hwan Yong Choi, Kyung Woo Kim. Writing - original draft: Min Hee Heo, Hwan Yong Choi. Writing - review & editing: Min Hee Heo, Hwan Yong Choi, Ji Yeon Kim, Kyung Woo Kim, Sang Il Lee. Supervision: Kyung-Tae Kim, Won Joo Choe, Jun Hyun Kim. Validation: Jang Su Park.
REFERENCES
1. HIP ATTACK Investigators. Accelerated surgery versus standard care in hip fracture (HIP ATTACK): an international, randomised, controlled trial. Lancet 2020; 395: 698-708.

2. Smith EB, Parvizi J, Purtill JJ. Delayed surgery for patients with femur and hip fractures-risk of deep venous thrombsis. J Trauma 2011; 70: E113-6.

3. Kim KK, Lee SW, Choi JK, Won YY. Epidemiology and postoperative complications of hip fracture during COVID-19 pandemic. Osteoporos Sarcopenia 2022; 8: 17-23.



4. Sakr Y, Giovini M, Leone M, Pizzilli G, Kortgen A, Bauer M, et al. Pulmonary embolism in patients with coronavirus disease-2019 (COVID-19) pneumonia: a narrative review. Ann Intensive Care 2020; 10: 124.




5. Konstantinides SV, Meyer G, Becattini C, Bueno H, Geersing GJ, Harjola VP, et al. 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS). Eur Heart J 2020; 41: 543-603.


6. Zhang Z, Shen B, Yang J, Zhou Z, Kang P, Pei F. Risk factors for venous thromboembolism of total hip arthroplasty and total knee arthroplasty: a systematic review of evidences in ten years. BMC Musculoskelet Disord 2015; 16: 24.




7. Roncon L, Zuin M, Barco S, Valerio L, Zuliani G, Zonzin P, et al. Incidence of acute pulmonary embolism in COVID-19 patients: Systematic review and meta-analysis. Eur J Intern Med 2020; 82: 29-37.



8. Huang CB, Hong CX, Xu TH, Zhao DY, Wu ZY, Chen L, et al. Risk factors for pulmonary embolism in ICU patients: a retrospective cohort study from the MIMIC-III database. Clin Appl Thromb Hemost 2022; 28: 10760296211073924.


9. Mir├│ ├Æ, Jim├®nez S, Mebazaa A, Freund Y, Burillo-Putze G, Mart├Łn A, et al. Pulmonary embolism in patients with COVID-19: incidence, risk factors, clinical characteristics, and outcome. Eur Heart J 2021; 42: 3127-42.



10. Bikdeli B, Madhavan MV, Jimenez D, Chuich T, Dreyfus I, Driggin E, et al. COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up: JACC state-of-the-art review. J Am Coll Cardiol 2020; 75: 2950-73.


11. Jarvis S, Salottolo K, Madayag R, Pekarek J, Nwafo N, Wessel A, et al. Delayed hospital admission for traumatic hip fractures during the COVID-19 pandemic. J Orthop Surg Res 2021; 16: 237.




12. Tripathy SK, Varghese P, Panigrahi S, Panda BB, Velagada S, Sahoo SS, et al. Thirty-day mortality of patients with hip fracture during COVID-19 pandemic and pre-pandemic periods: A systematic review and meta-analysis. World J Orthop 2021; 12: 35-50.



13. Villa JM, Pannu TS, Piuzzi NS, Krebs V, Riesgo AM, Higuera CA. A major increase of thromboembolic events in total hip and knee arthroplasty patients during the COVID-19 pandemic. Hosp Pract (1995) 2022; 50: 68-74.


-
METRICS

-
- 1 Crossref
- 1,548 View
- 36 Download
- Related articles in Anesth Pain Med
-
Liver transplantation of a patient with extreme thrombocytopenia - A case report -2021 July;16(3)
- ARTICLE & TOPICS
-
- Topics
-
- Neuroscience in anesthesiology and critical care
- Anesthetic Pharmacology
- Obstetric Anesthesia
- Pediatric Anesthesia
- Cardiothoracic and Vascular Anesthesia
- Transplantation Anesthesia
- Spinal Pain
- Regional Anesthesia
- Neuromuscular Physiology and Pharmacology
- Airway Management
- Geriatric anesthesia and Pain
- Others