Single puncture combined lumbar erector spinae plane and quadratus lumborum block (SEQ block) in acetabular fracture surgeries: randomized clinical trial
Article information
Abstract
Background
Acetabular fracture surgery can cause severe postoperative pain. A combined lumbar erector spinae plane block and paraspinous sagittal shift quadratus lumborum block may augment analgesia.
Methods
Fifty two patients undergoing posterior column acetabular surgery were divided into: Group Single puncture combined lumbar Erector spinae and Quadratus lumborum block (SEQ): patients who received SEQ block before anesthesia; and Group morphine (MOR), those who received general anesthesia (GA) and morphine.
Results
Demographic characteristics were comparable. The heart rate and mean arterial blood pressure were significantly lower in the SEQ group than in the MOR group between 60 and 180 min intraoperatively (P < 0.001). Postoperative resting and dynamic visual analogue scale scores in the SEQ group were significantly lower than those in the MOR group at all studied periods (P = 0.022–0.001), except at 20 and 24 h postoperatively. Fentanyl was required in all MOR group patients at a mean dose of 110.0 ± 28.42 µg while 18 patients required fentanyl in SEQ group at a mean dose of 60.55 ± 25.54 µg. Postoperative morphine consumption was significantly less in SEQ group (6.33 ± 2.37 mg) than MOR group (17.0 ± 2.55 mg). Postoperative nausea and vomiting were recorded in eight and four patients in MOR and SEQ group, respectively. No complications associated with the block technique were observed.
Conclusions
The SEQ block reduces the postoperative opioid consumption and provides stable intra and postoperative hemodynamics without observed complications in posterior column acetabular surgery.
INTRODUCTION
Acetabular fractures are uncommon and occur less frequently than upper or lower limb fractures. However, these fractures are usually disabling because they progressively impair the articular surfaces of the hip joints. Fixation of such fractures usually requires an aggressive surgical technique; consequently, postoperative pain may be significant, resulting in delayed rehabilitation and prolonged hospital stay. The opioids required to control pain are often associated with undesirable sedation, nausea, and vomiting, which may limit active postoperative physical therapy [1]. Epidural analgesia when compared with opioid-based analgesia, epidural analgesia does not enhance analgesia, postoperative rehabilitation, or physical therapy [2].
The lumbar and sacral plexuses are involved in the acetabular innervation. The dorsal rami of the lumbar nerve roots provide a surgical incision during the posterior surgical approach for acetabular fractures [1]. Multiple injections are typically required to achieve adequate regional analgesia during acetabular surgery. We suggest a novel approach for combined lumbar erector spinae plane block (ESPB) and paraspinous sagittal shift quadratus lumborum (PSSS QL) block for perioperative analgesia in hip/acetabular surgeries using a single-puncture technique (SEQ block).
Aim of the study
The primary aim of this study was to compare the total postoperative opioid (morphine) consumption after posterior column acetabular surgery when providing ultrasound guided SEQ block: single puncture combined lumbar ESPB and PSSS QL block versus conventional intravenous morphine analgesia.
The secondary aims of this study were to assess intraoperative and postoperative mean arterial pressure (MAP) and heart rate (HR), resting visual analogue scale (VAS) score, dynamic VAS score, and postoperative complications.
MATERIALS AND METHODS
This prospective randomized study was reviewed and approved by the University Local Ethics Committee of Egypt (IRB no. 00007555) and a written informed consent was obtained from each patient for participation in the study. The trial was conducted in the period between January 2021 and January 2022. The trial adhered to the principles of the Declaration of Helsinki and complied with CONSORT for reporting of randomized clinical trials. The study was registered in the Clinical Trials Registry prior to patient enrollment (NCT04688814; date of registration: December 25, 2020). This study was conducted starting from December 30, 2020, for 1 year on American Society of Anesthesiologists physical status I-III patients scheduled for unilateral posterior wall/column acetabular fracture surgery using the posterior approach. The exclusion criteria were body mass index > 35 kg/m2, pre-existing neurological deficits, spinal deformity, pregnancy/lactation, significant renal or hepatic impairment, known contraindications to peripheral nerve block (coagulopathy or infection at the site of injection), or chronic opioid users/abusers.
During the study period, 58 patients were screened for recruitment. Two patients did not meet the inclusion criteria, and four refused to participate in the study (Fig. 1). Fifty-two patients completed the study and were randomly divided into two groups using a closed envelope method via a simple randomization sheet: Group SEQ Patients received an ultrasound-guided SEQ block preoperatively before the induction of general anesthesia (GA); And Group MOR Patients received GA and analgesia was based on opioids mainly intravenous morphine.
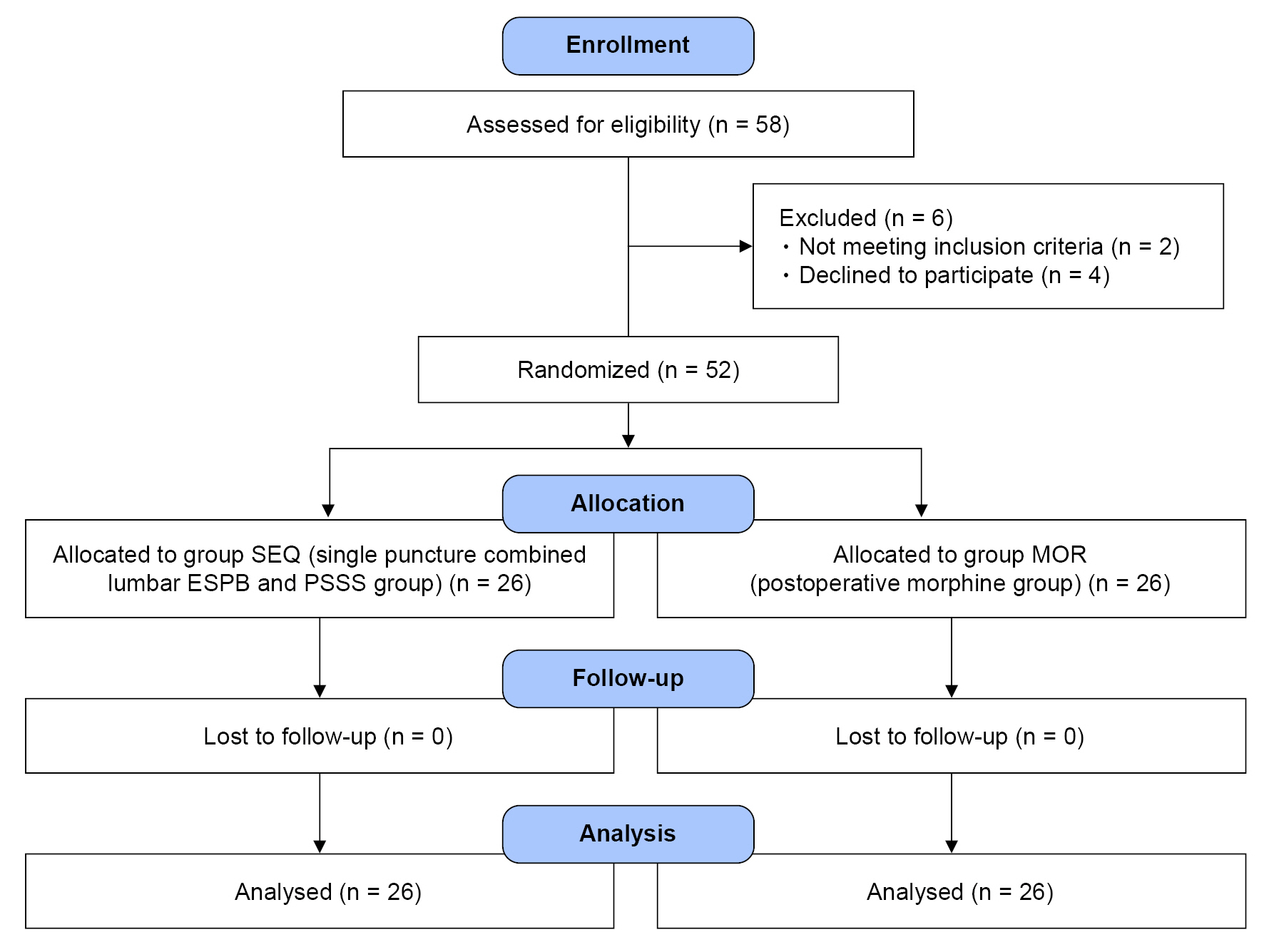
Consort flow diagram. SEQ: Single puncture combined lumbar Erector spinae and Quadratus lumborum block, MOR: morphine.
Upon arrival at the block room, a multichannel monitor was attached to the patients, followed by the administration of 2 mg midazolam IV after securing an IV cannula.
SEQ block
This is a combination of the PSSS QL block and the ESPB. Before the induction of GA in the SEQ group, the patients were placed laterally on the healthy side with the fracture side independent (Figs. 2, 3). A curvilinear ultrasound transducer (2–5 MHz) (Versana active 1.5, GE medical systems, China) was placed in a parasagittal plane 3–4 cm lateral to the lumbar spinous process of L4 (which is almost opposite to the iliac crest), producing a longitudinal scan of the lumbar paravertebral region, thus identifying the transverse processes of L3 and L4 with psoas muscle (PM) in-between and erector spinae muscle (ESM) posteriorly (superficial to transverse processes). The probe was shifted slowly to the lateral side until the transverse processes disappeared and QL muscle was evident in its long axis attached caudally to the iliac crest with a characteristic sonographic image of three muscle layers appearing from posterior to anterior as the ESM, QL, and PM muscles. The anterior layer of the thoracolumbar fascia (ATLF), which is considered to be a continuation of fascia transversalis, separates the PM and QL muscles.
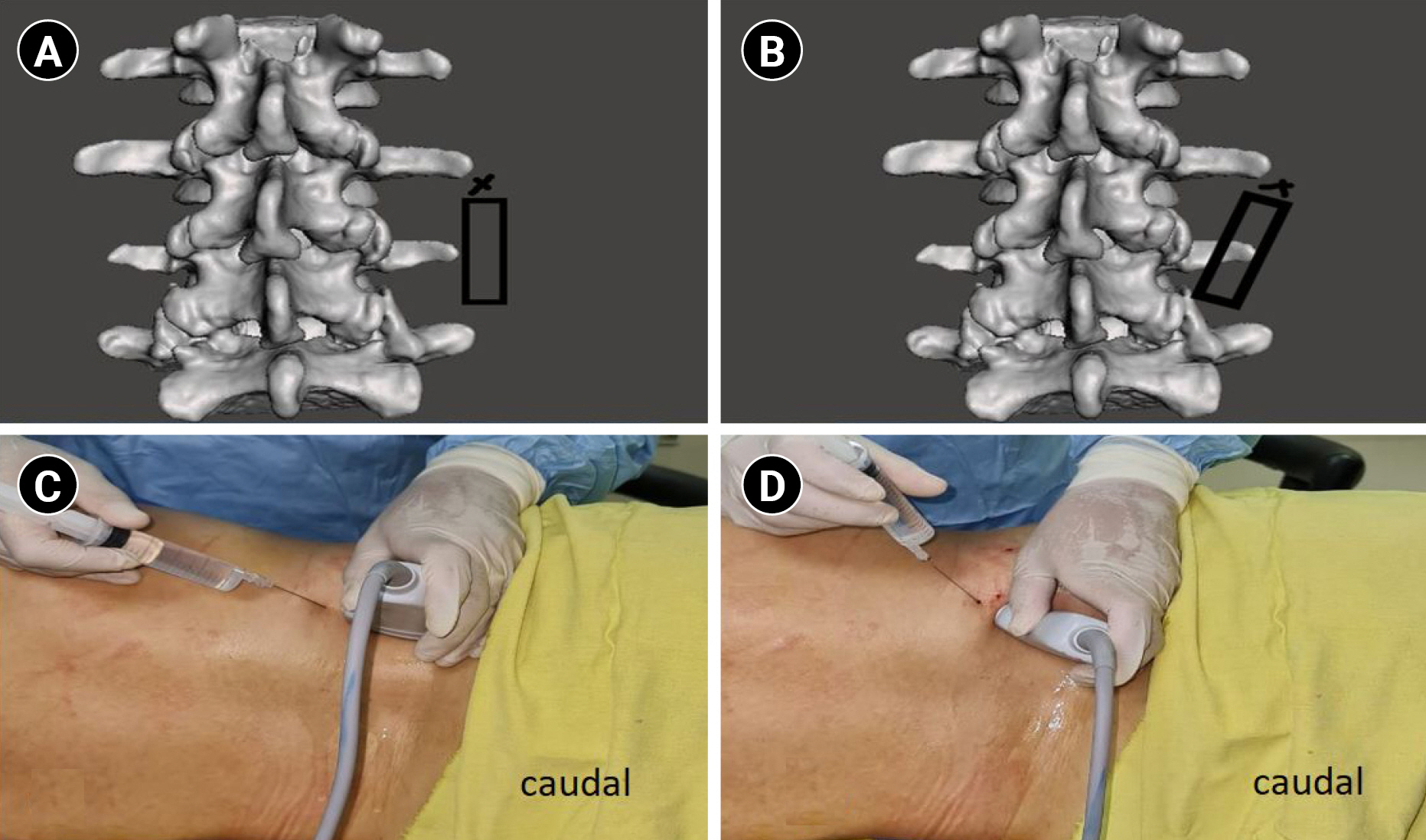
Probe position during SEQ block technique. (A) Probe in the parasagittal plane about 4 cm lateral to the lumbar vertebrae spinous processes with needle entry point at the cephalic end of the probe; (B) caudal end of the probe has been rotated medially towards the lumbar spine until the hypoechoic shadow of the transverse process of L4 appears in the ultrasound image; (C) probe position corresponding to (A); (D) probe position corresponding to (B). SEQ, Single puncture combined lumbar Erector spinae and Quadratus lumborum block.

Real ultrasound image of the steps of SEQ block. (A) Probe position about 4 cm parallel to lumbar vertebrae with transverse processes appearing in view; (B) characteristic sonographic image of three muscle layers from posterior to anterior: erector spinae, quadratus lumborum and psoas major muscle: (C) PSSS QL block, red arrow represents needle path to the endpoint of injection into the plane between QL and PM muscles in a craniocaudal direction with LA spreading caudally; (D) lumbar ESP block after the caudal end of the probe is rotated medially, here, transverse process of L4 appears in view. The red arrow represents needle path towards transverse process of L4. SEQ: Single puncture combined lumbar Erector spinae and Quadratus lumborum block, PSSS: paraspinous sagittal shift, QL: quadratus lumborum, PM: psoas muscle, LA: local anesthetic, ESP: erector spinae plane, ES: erector spinae muscle, Psoas: psoas major muscle, tr pr L4: transverse process of lumbar vertebra 4, tr pr L5: transverse process of lumbar vertebra 5.
After subcutaneous local infiltration with lidocaine 1% at the cephalic end of the probe, the block needle was advanced in the cephalo-caudal direction, through the ES and QL muscles, until it pierced the epimysium of the QL muscle. Local anesthetic (LA) was injected anterior to the QL, and its spread was observed in a caudal direction towards the iliac crest in the plane between the QL and psoas muscles.
The caudal end of the probe was then rotated slowly medially towards the lumbar spine until a hypoechoic shadow of the transverse process of L4 appeared on the ultrasound image. The needle was withdrawn into the subcutaneous tissue and advanced in the plane towards the transverse process of L4. After contact, the LA was deposited in the plane between the transverse process and the overlying ESM. Total volume of LA used was 50 ml of 0.25% bupivacaine, 25 ml for each injection.
The patients were transported to the operating room where general anesthesia was induced. No blocks were administered in the MOR group.
Anesthesia was induced with propofol (2 mg/kg), atracurium (0.5 mg/kg), and fentanyl (1 µg/kg), followed by endotracheal intubation. Anesthesia was maintained with isoflurane 1 MAC in 60% oxygen. The multimodal analgesic protocol included the intravenous administration of dexamethasone (8 mg), paracetamol (1 g), and ketorolac (60 mg). Increments of 0.5 µg/kg of fentanyl were administered intraoperatively if there was an increase in HR/MAP above 20% of the basal value.
Postoperatively, a multimodal analgesic regimen was continued in the form of paracetamol 1 g/8 h and ketorolac 30 mg/8 h intravenously for 48 h. Intravenous morphine in a dose of 0.05 mg/kg was given as a rescue analgesic when the VAS was ≥ 4.
Postoperatively, the assessment was performed by an investigator blinded to the group allocation. HR and MAP were recorded preoperatively (baseline) and every 30 min during surgery, and at 1, 2, 4, 8,12, 16, 20 and 24 h postoperatively. Resting and dynamic VAS scores were recorded every hour for the first 4 h and then every 4 h for the remaining 24 h during postoperative follow-up. Total analgesic requirements in the form of intraoperative fentanyl and postoperative morphine were measured. Complications associated with the block technique and the opioids have also been documented.
Statistical analysis
Sample size was calculated using G-power software, considering power 80%, level of confidence 95% and effect size 0.701 based on the required dose of morphine in a previous study [1], in which group 1 required 6 mg (0–14 mg), while group 2 required 10 mg (2–16 mg). The total sample size was 52 patients (26 in each group).
Data were collected and statistical analysis was performed using the Statistical Package for Social Sciences (version 24.0, SPSS Inc.). Numerical data were compared using the unpaired t-test, and categorical variables were analyzed using the chi-square test. Data are presented as mean ± standard deviation, or as a number (proportion), and the effect was considered statistically significant at P < 0.05.
RESULTS
Fifty-two patients were included in the study and were divided into two groups (26 each): MOR and SEQ. There were no significant differences between the two groups in terms of patient demographics, comorbidities, or duration of surgery (Table 1). HR and MAP were significantly lower in the SEQ group than in the MOR group starting from 60 min to 180 min intraoperatively (P < 0.005 to < 0.001) (Fig. 4). There was no significant difference between the two groups postoperatively regarding the same parameters, except at 8, 12, 20 and 24 h postoperatively, when the HR was significantly lower in the SEQ group than in the MOR group (P = 0.031, 0.043, 0.044, and 0.002, respectively). Postoperative resting VAS score was significantly lower in the SEQ group than in the MOR group in all studied periods, with P value ranging from 0.003 to 0.001, except at 20 and 24 h postoperatively (P = 0.603, 0.544 respectively). The dynamic VAS score in the SEQ group was less significantly than that in the MOR group during the entire postoperative study period, with P values ranging from 0.022 to 0.001, except at 20 h and 24 h (P was 0.891 and 0.167 respectively) (Fig. 5). Fentanyl was required in all cases of the MOR group intraoperatively at a mean dose of 110.0 ± 28.42 µg while 18 patients required intraoperative fentanyl in the SEQ group at a mean dose of 60.55 ± 25.54 µg. Postoperative morphine consumption was significantly less in the SEQ group than MOR group. The mean dose of morphine was 6.33 ± 2.37 mg in SEQ patients relative to 17.0 ± 2.55 mg in MOR patients (Table 2). Postoperative nausea and vomiting were recorded in eight patients in the MOR group and four patients in the SEQ group with no significant differences between the two groups. No complications associated with the block technique were observed.

Comparison of the intra-operative and post-operative hemodynamics between the two groups. MOR: morphine, SEQ: Single puncture combined lumbar Erector spinae and Quadratus lumborum block, BP: blood pressure, HR: heart rate. *P < 0.05 was considered statistically significant.
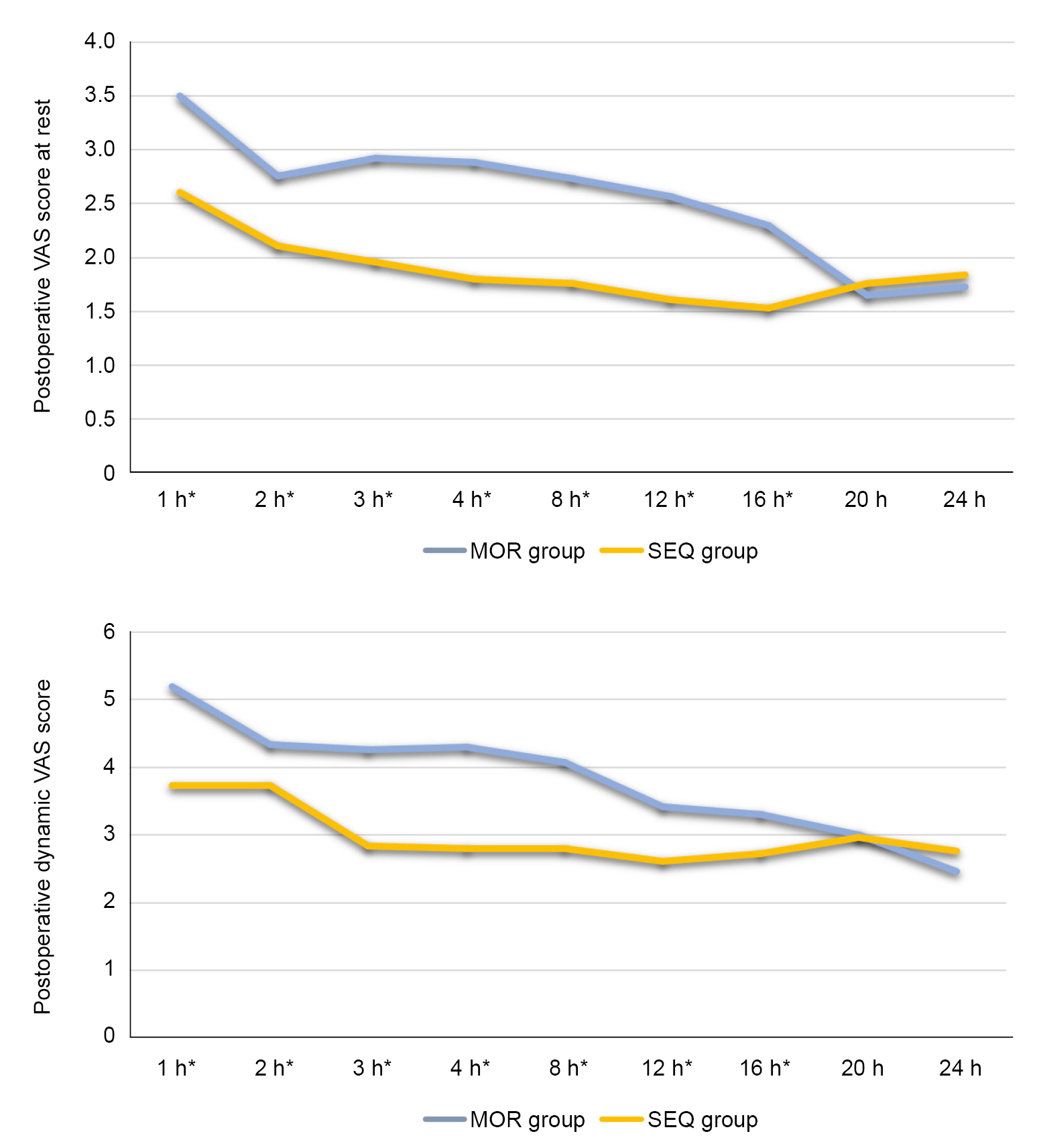
Comparison between of the resting and dynamic VAS scores between the two groups. MOR: morphine, SEQ: Single puncture combined lumbar Erector spinae and Quadratus lumborum block, VAS: visual analogue scale. *P < 0.05 was considered statistically significant.
DISCUSSION
Recent advances in regional anesthesia are extremely beneficial for acetabular surgery associated with extensive dissection and deep tissue trauma. Epidural and psoas compartment blocks were used. However, these techniques are associated with technical difficulties and obstacles associated with anticoagulation therapy [1,2]. Moreover, a few case series have discussed other regional anesthetic techniques such as the supra-inguinal fascia iliaca compartment block [3] and the pericapsular nerve group block [4], in the anterior approach for acetabular fractures.
The SEQ block significantly reduced the postoperative opioid consumption and improved both the resting and dynamic VAS scores in patients who underwent posterior column acetabular surgery. To the best of our knowledge, no previous studies have evaluated the effectiveness of combining a QL block and the lumbar ESPB in acetabular fracture surgery. The current technique of combining the two blocks involves a single skin puncture; therefore, it may carry a lower risk of patient’s discomfort and a lower possibility of tissue trauma.
Recently, much research has been conducted to examine the reliability of either the lumbar ESPB or the QL block alone in providing adequate postoperative analgesia for hip surgery patients. The ESPB is one of the most recent plane blocks and is still extensively evolving in research and clinical practice, with only a few studies on its application at the lumbar level. Lumbar ESPB has been studied in the literature for many indications such as chronic low back pain, spinal surgery, herpes and lower extremity surgery [5-8]. To date, debate still exists regarding the mechanism of action, LA spread, and the volume and type of injectate of either block, with inconsistent results. The anatomic spread of LA in lumbar ESPB has been reported to spread craniocaudally between T12 and S1 posterior to the transverse processes with significant anterior spread to the lumbar neural foramina and lumbar plexus [9] Tulgar et al. [10] demonstrated caudal spread towards the highest part of the sacral plexus with anterior and posterior spread surrounding the psoas major muscle and lumbar plexus. An Injection of 40 ml resulted in LA spreading to the anterior and posterior epidural spaces, as demonstrated by magnetic resonance imaging [6]. Ahiskalioglu et al. [8] reported adequate anesthesia in 15 high-risk elderly patients who underwent hip surgery with lumbar ESP combined with mild sed-analgesia. One cadaveric study demonstrated variable anatomic spread to different lumbar levels with a fixed LA volume of 20 ml. In addition, the anterior spread varied, with infrequent spread to the lumbar nerve roots [11]. Another cadaveric study reported no anterior LA spread in any of the examined specimens [12].
Several previous case reports and a few randomized clinical trials have been conducted to evaluate the efficacy of the quadratus lumborum block as a part of a multimodal analgesic technique to improve postoperative analgesia in patients undergoing hip surgery; however, only case reports have discussed its use in acetabular surgery [13-15]. The psoas major muscle lies ventromedial to the QL muscle, housing the lumbosacral plexus [16]. Most previous studies have demonstrated consistent LA spread to the L1-3 nerve roots [17]. The same authors of the current study developed a modification of the transmuscular QL block called the PSSS QL block which was examined in four cases of hip surgery. The spread of the injectate was confirmed via an A-P fluoroscopic imaging of the lumbosacral spine after injection of a mixture of LA and contrast. The epimysium of the QL was pierced and the LA was deposited into the plane between the psoas major and the QL muscle under fascia transversalis (ATLF) at the level of L4. Fluoroscopic imaging confirmed the spread of the LA in the course of the PM muscle towards the pelvis beyond the level of the 5th lumbar vertebra with medial spread towards the lumbar nerve roots in the lumbar paravertebral region [18]. The same QL block technique was used in the 1st step of this study.
The two blocks are suggested to augment each other with the possibility of providing more caudal blockade via the lumbar ESPB through the spread of the LA to the highest parts of the sacral plexus and cluneal nerves, which may provide more potent analgesia in patients undergoing acetabular surgery. The results of the current study demonstrated significantly lower intra-and postoperative opioid requirements with a reduction in VAS scores at rest and during movement and more stable postoperative hemodynamics. Eight patients in the SEQ group did not require rescue analgesia during the first 24 h postoperative period.
SEQ has several advantages. The endpoint of injection is the fascial plane rather than a specific motor response required during lumbar plexus stimulation, which allows easy identification while avoiding the possible risks of nerve injury, inadvertent dural puncture, and intrathecal spread of the LA. The injectate is allowed to spread caudally and may reach the plane under the fascia iliaca and also the upper branches of the sacral plexus, with the PM muscle providing a protective barrier against accidental needle entry into the peritoneal cavity.
The current study had several limitations. Spread of the injectate was not confirmed neither radiologically nor by examination of the sensory level before anesthesia. This is prevented by patient positioning and operative theatre turnover. A motor assessment of the block was not performed; however, none of the patients complained of motor weakness during rehabilitation on the first postoperative day. The lack of a single-block control group did not allow for a precise judgment of the advantages of combining the two blocks. Nevertheless, these results are promising and encouraging. Further research is required to accurately determine the advantages of adding lumbar ESPB to the PSSS-QL block during hip surgery.
The present study concluded that single puncture lumbar ESPB and PSSS QL blocks (SEQ block) reduced the postoperative opioid consumption and provided stable intra-and postoperative hemodynamics without any observed complications in posterior column acetabular surgeries.
Notes
FUNDING
None.
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
DATA AVAILABILITY STATEMENT
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
AUTHOR CONTRIBUTIONS
Data curation: Moustafa Abdelaziz Moustafa. Formal analysis: Aly Mahmoud Moustafa Ahmed. Methodology: Moustafa Abdelaziz Moustafa, Ahmad Samir Alabd. Project administration: Ahmad Samir Alabd. Visualization: Aly Mahmoud Moustafa Ahmed. Writing - original draft: Moustafa Abdelaziz Moustafa, Ahmad Samir Alabd. Writing - review & editing: Moustafa Abdelaziz Moustafa. Investigation: Aly Mahmoud Moustafa Ahmed. Supervision: Ahmad Samir Alabd. Validation: Aly Mahmoud Moustafa Ahmed.


