Quadriplegia as a position-related complication after parotidectomy: the need for cooperation between anesthesiologists and surgeons when positioning patients - A case report -
Article information
Abstract
During surgery, the patient is positioned optimally according to the type of operation. Careful attention is required because damage associated with patient positioning may occur during the course of the surgery. Here, we present a case of hyperextension neck injury observed following parotidectomy. A 68-year-old man who was diagnosed with a parotid tumor underwent an elective right partial superficial parotidectomy. After surgery, the patient was not able to move his upper and lower extremities and experienced voiding difficulty. Cervical magnetic resonance imaging showed spinal cord injury at the C3-4 and C5-6 levels. High-dose steroid treatment was started, and emergency laminoplasty C4-5 to C5-6 was performed. Following laminoplasty, motor function was almost fully recovered, but proprioception was weak, and voiding difficulty remained a problem. The patient received rehabilitation treatment in the hospital for about 3 months, demonstrating improvement. He was discharged and continued treatment in the outpatient department.
INTRODUCTION
Peripheral nerve damage associated with patient positioning occurs not infrequently. However, quadriplegia following non-spinal surgeries is a rare complication. Several reports claim injury resulting from hyperextension of the cervical spine. Most of these cases were related to pre-existing cervical spondylosis and cervical spinal stenosis, in which the spinal cord was vulnerable to damage caused by prolonged neck extension. Compression of the cervical spinal cord can lead to sequelae such as diminished fine motor skills of the hand or balance difficulties, or incontinence and complete paralysis in severe cases. We present a case of quadriplegia caused by prolonged neck hyperextension during the performance of parotidectomy and discuss reasons for cervical cord injury in similar cases.
CASE REPORT
A 68-year-old man who weighed 73 kg and was 164 cm tall visited the otorhinolaryngology department for evaluation of pain that he had experienced on the right side of his face for the previous 4 years. Neck computerized tomography (CT) could not rule out abscess or a tumorous condition. The patient was scheduled to undergo right partial superficial parotidectomy. According to preoperative evaluation, his other medical conditions included hypertension, diabetes mellitus, and stable angina pectoris. Two-dimensional and Doppler echocardiogram and electrocardiogram (ECG) revealed no abnormal findings with the exception of multiple premature ventricular contractions. Chest radiography, pulmonary function tests, and laboratory tests showed no abnormalities. An 18-gauge intravenous line was inserted in the right arm, and lactated Ringer’s solution was infused. The patient entered the operating room without premedication. Oxygen saturation (SpO2), non-invasive blood pressure (NIBP), and ECG were monitored. The patient’s initial vital signs were: NIBP, 140/76 mmHg; SpO2, 99%; and heart rate, 88 beats/min. Preoxygenation with 100% oxygen was applied. Pentothal sodium 350 mg, 2% lidocaine 4 ml, and rocuronium 50 mg were injected for induction of anesthesia. Mask ventilation was applied with 50% oxygen, 50% N2O, and 4 vol% sevoflurane. In 3 minutes, the patient was gently intubated with an 8.0 mm cuffed reinforced endotracheal tube. Anesthesia was maintained with 2 volume% sevoflurane and N2O. Invasive arterial blood pressure was monitored at the left radial artery.
After induction of general anesthesia, the patient was positioned supine, and a surgical pad was placed under the shoulders to create extension of the neck. He did not undergo urinary catheterization. To avoid damage to the facial nerve, nerve stimulator monitoring was applied.
The operation was completed uneventfully in about 5 hours. Intraoperative vital signs were maintained stable: systolic blood pressure, 110–90 mmHg; SpO2, 99%; heart rate, 62–52 beats/min; and body temperature, 35–36.0°C. The total fluid input was 1,100 ml crystalloid and the estimated blood loss was minimal. The patient recovered from general anesthesia in the post anesthesia care unit (PACU) for an hour and then moved to the general ward.
In the ward, urine was removed using a Nelaton catheter because the patient did not void during the operation. At 4 hours postoperatively, he remained unable to void, and the Nelaton catheter was applied again. The Nelaton catheter was applied twice more after that. At 8 hours postoperatively, the patient reported that he could not move his extremities. Motor level was checked using manual muscle testing with grading according to the Medical Research Council scale (Table 1) [1]. The upper and lower limb muscle strength on the left side were grade 3/5 and 1/5, and those on the right side were grade 3/5 and 2/5, respectively. Under suspicion of cerebral infarction, brain magnetic resonance imaging (MRI) was performed; this showed no acute lesions. Cervical MRI was performed and confirmed compressive myelopathy at the C3-4 and C5-6 levels, indicating spinal cord injury (Fig. 1). High-dose steroid treatment was started (methylprednisolone 62.5 mg was given every 6 hours intravenously) and emergency laminoplasty C4-5 to C5-6 was performed at 20 hours after parotidectomy. Immediately after emergency laminoplasty, the patient’s motor function was grade 4/0 on the left side and grade 4/1 on the right side, and the urinary retention persisted. At 3 days postoperatively, muscle strength was improved to grade 4/4 on the left side, and grade 4/4+ on the right side. With 3 months of rehabilitation, the patient’s muscle strength improved to grade 5/4+ on the left side and 5/4+ on the right side, but the proprioceptive impairment had not fully improved. He was discharged at 102 days postoperatively. At 6 months postoperatively, the patient can walk but has a little difficulty maintaining his balance, and there is no urinary retention.

Grading System of Manual Muscle Testing according to Medical Research Council Scale. Procedure to Evaluate the Function and Strength of Muscles according to Gravity and Manual Resistance
DISCUSSION
Several cases of hyperextension injury during non-spinal surgery have been reported in the literature: coronary artery bypass surgery (CABG), parathyroidectomy, thyroidectomy, thyroid biopsy, stapedectomy, adenotonsillectomy, and dental extraction.
Quadriplegia has been related to long-term hemodialysis [2,3], asymptomatic or undiagnosed cervical spondylosis or herniated disc [4-8], cervical meningioma [9], symptomatic cervical spondylosis [10], and undetected atlanto-axial instabililty [11] according to a review of the literature.
These kinds of operations, such as CABG and parathyroidectomy, require prolonged hyperextension. Most cases of reported prolonged neck extension might include predisposing factors contributing to spinal cord injury, such as asymptomatic or undiagnosed cervical spondylosis or herniated disc, or long-term hemodialysis. Because these surgeries commonly have durations of 4 to 5 hours, operating time is not simply a risk factor but could be a possible contributor to injury in the patient with pre-existing cervical disease.
Long-term hemodialysis is associated with extradural amyloid deposition. Destructive spondyloarthropathy (DSA) has been reported frequently as a consequence of amyloid deposition. DSA can potentially cause myelopathy or radiculopathy because of amyloid deposits within the disc and peridiscal ligaments [12]. Extradural amyloid deposition is likely to contribute to cervical stenosis. Two patients undergoing parathyroidectomy [3] and 1 undergoing CABG [2] were receiving long-term hemodialysis. Extradural deposition of amyloid might cause cervical spinal canal stenosis before surgery but the condition could be asymptomatic, and the cervical cord might additionally be compressed by neck hyperextension for surgical exposure.
There were several cases of hyperextension injury associated with CABG in the literature: 4 cases related to undiagnosed or asymptomatic cervical spondylosis [4-6,8], 1 case related to undiagnosed cervical disc herniation [7], 1 case with previous cervical spondylosis [10], and 1 case with hemodialysis associated with extradural amyloid deposition and cervical spondylosis [2]. Cervical cord injury might be induced by aggravating pre-existing spinal canal stenosis during surgery. Furthermore, these reports suggested that extension of the neck should be avoided in patients with cervical spine stenosis. In particular, elderly patients should be advised to undergoing screening for cervical spine stenosis, and informed before surgery of the possibility of the development of neurologic deficits.
Cervical spondylosis is age-related degenerative changes that may affect vertebrae, discs, facet joints, and ligaments. A study reported that on lateral cervical radiography, degenerative changes were found on 1 or more levels in 70% of women and 95% of men among 200 asymptomatic individuals 60 to 65 years old [13]. Another study of 63 asymptomatic individuals without cervical disease showed that almost 60% of those older than 40 years had degenerative change and disc space narrowing at 1 or more levels on cervical spine MRI [14]. Among patients with preexisting cervical spondylosis, increases in spinal stenosis and significant narrowing of the subarachnoid space were observed after neck extension compared with neutral position in 48% [15]. Although the patient in the current case had not reported neck pain before surgery, we assumed that he had asymptomatic cervical spondylosis, and the prolonged hyperextension during the surgery aggravated the spinal stenosis. Retrospectively, we rechecked the neck CT image that was obtained before parotidectomy. On that image, we were able to recognize the presence of cervical spondylosis with ossification of the posterior longitudinal ligament (Fig. 2).
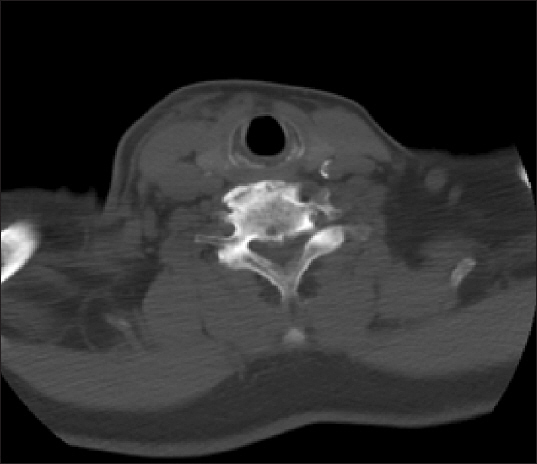
Neck computed tomography obtained before parotidectomy. Image shows cervical spondylosis and ossification of posterior longitudinal ligament.
In the present case, it took 8 hours to recognize the patient’s neurological deficits. Because we had no previous experience with hyperextension injury, we did not consider that neurological impairment might occur. Therefore, we suggest that patients with risk factors for hyperextension injury should be examined for neurological function in the PACU.
To avoid hyperextension injury, we suggest careful evaluation of the cervical spine before high risk surgeries such as CABG, thyroidectomy, parathyroidectomy, and parotidectomy that require prolonged neck hyperextension, especially in patients with risk factors such as neck pain with cervical spondylosis, herniated cervical disc, advanced age, or long-term hemodialysis for end-stage renal disease. In head and neck surgery, hyperextension and turning of the head to the opposite side are recommend. Proper visibility is also important, but it is expected that appropriate standards will be maintained.
The most important lessons in our case are that anesthesiologists should keep in mind the possibility of hyperextension injury and should put their best effort into preventing this injury. For anesthesiologists, supreme effort is needed to avoid excessive neck extension during intubation and positioning. The surgical team should also be conscious of the possibility of the development of neurologic deficits owing to patient positioning. If possible, release of neck hyperextension a few times during surgery is highly recommended. Therefore, cooperation between anesthesiologists and surgeons is required during positioning of patients. Immediate examination and treatment are also essential when neurological symptoms occur.
