Trigeminocardiac reflex: sudden severe bradycardia during open reduction for temporomandibular joint dislocation - A case report -
Article information
Abstract
Background:
The trigeminocardiac reflex (TCR), which occurs after stimulation of the territory of the trigeminal nerve, is very rarely reported to be caused by stimulation of the mandibular branch. We report a case of TCR in open reduction for temporomandibular joint (TMJ) dislocation.
Case:
A 74-year-old female presented for TMJ dislocation. During open reduction of TMJ under general anesthesia, severe bradycardia (15 beats/min) occurred. Immediately 0.5 mg atropine was administered intravenously, and the surgical manipulation was stopped. After 30 seconds, heart rate normalized. During surgery, severe bradycardia occurred one more time. It disappeared spontaneously as soon as surgical manipulation was stopped. The surgery was completed uneventfully.
Conclusions:
Because of the possibility of profound bradycardia, asystole, or even death when evoked, it is important to be aware of the trigeminocardiac reflex during manipulation of the mandibular divisions, especially during surgical stimulation of the TMJ.
The trigeminocardiac reflex (TCR) manifests as bradycardia or asystole with hypotension when any branch of the trigeminal nerve is stimulated [1]. The oculocardiac reflex (OCR) is a subtype of the TCR, which has commonly been reported during extraocular muscle surgery [2–6]. Severe bradycardia and cardiac arrest also have been observed during cases of division II surgery such as maxillectomy, zygomatic arch surgery, and repositioning maxillary fractures [1,7]. However, there have been few reports of such cases during division III surgery [1]. Although this complication occurs only rarely, every craniomaxillofacial surgeon and anesthesiologist should be aware of the possibility of this severe phenomenon.
Here we report a case of severe bradycardia due to TCR occurring during surgical reduction for persistent temporomandibular joint (TMJ) dislocation.
CASE REPORT
A 74-year-old woman (156 cm, 51 kg) presented to a dental clinic for bilateral TMJ dislocation. The onset of TMJ dislocation was unknown. The patient could not eat properly because of the TMJ pain, and required dentures owing to lack of any teeth. Therefore, closed reduction for TMJ dislocation under monitored anesthesia care was planned. The patient had no history of trauma or medical illness, with the exception of Alzheimer’s disease. Preoperative electrocardiographic findings showed normal sinus rhythm (heart rate [HR] 65 beats/min) and premature ventricular contractions. Other routine preoperative laboratory tests and chest radiographs showed values within the normal range. The patient showed no cardiac signs or symptoms.
Under monitored anesthesia care with propofol and remifentanil, closed reduction for TMJ dislocation was attempted. However, closed reduction failed owing to severe lateral pterygoid muscle contracture resulting from long-term TMJ dislocation.
Three days later, open reduction under the general anesthesia was scheduled and additional preoperative echocardiography and pulmonary function tests were performed. There were no abnormalities on echocardiogram or pulmonary function tests. The patient was premedicated with glycopyrrolate 0.2 mg intramuscularly. During general anesthesia, the patient was monitored with noninvasive blood pressure (NIBP), electrocardiogram, pulse oximetry, bispectral index (BIS), and end-tidal CO2 (ETCO2) concentration. Initial vital signs were stable, with blood pressure (BP) 120/70 mmHg and HR 71 beats/min. The patient was preoxygenated by face mask with 100% O2. After administration of lidocaine 40 mg, anesthesia was induced with intravenous propofol (target effect-site concentration [Ce], 3.5 μg/ml) and remifentanil (Ce, 3.5 ng/ml) with a target controlled infusion pump (Orchestra® Base Primea, Fresenius Kabi, Ltd., France) followed by rocuronium 40 mg. Anesthesia was maintained with intravenous propofol (Ce, 3–3.5 μg/ml) and remifentanil (Ce, 3–3.5 ng/ml) after flexible fiberoptic bronchoscopic guided nasotracheal intubation. Prior to the event, vital signs were stable at BP 95–135/65–85 mmHg and HR 65–80 beats/min. During the operation, BIS was maintained at 45–60, ETCO2 at 34–37 mmHg, and SpO2 at 97–100%. Prior to utilization of an extraoral approach, closed reduction was attempted because the muscle tension was reduced by the muscle relaxant. However, closed reduction failed because of fibrosis of the surrounding muscles and ligaments resulting from long-term dislocation of the TMJ.
For open reduction, 2% lidocaine containing 1 : 100,000 epinephrine was used for topical anesthesia in both mandibular areas followed by skin incision. After wiring in both mandibular angles, traction of the wires was performed (Fig. 1).
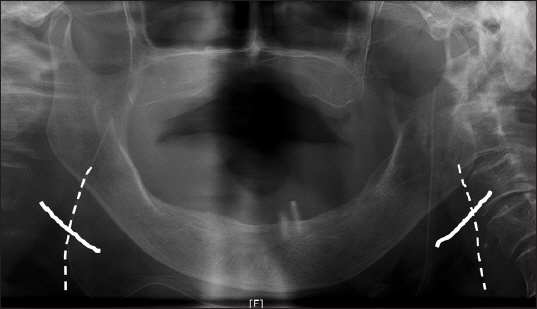
Postoperative panoramic view shows Incision and wiring. White lines: skin incisions in both mandibular areas, white dashed lines: wiring in both mandibular angles.
One hour and 30 min after induction of anesthesia, there was a severe bradycardia with a sudden decrease in HR from 74 beats/min to 15 beats/min during traction of the wire in the right mandibular angle. At that time, BP was 130/78 mmHg and hypotension did not occur. The surgical manipulation was immediately aborted, and 0.5 mg atropine was administered intravenously. After 30 seconds, the HR was normalized (HR 68 beats/min).
Thirty minutes after the event, severe bradycardia (HR 15 beats/min) occurred again during traction of the wire in the right mandibular angle. The bradycardia disappeared immediately upon termination of traction, with no pharmaceutical intervention.
After the bradycardia disappeared, the gentle and less strong traction was performed again, and there were no further bradycardia episodes. The operation time was 2 h and 50 min, and the anesthesia time was 3 h and 20 min. The surgery was completed uneventfully. The patient was discharged without any complications after two days.
DISCUSSION
The causes of intraoperative bradycardia include drug events, airway and ventilation problems, autonomic reflexes, and epidural anesthesia or spinal anesthesia [8]. In head and neck surgery, autonomic reflexes such as direct vagal stimulation, TCR or baroreceptor reflex can cause severe bradycardia, even cardiac arrest [4]. The most common cause of intraoperative bradycardia is a drug event [8]. However, in present case, the depth of anesthesia was maintained properly at BIS 45–60, vital signs were stable at BP 95–135/65–85 mmHg and HR 65–80 beats/min before the bradycardia event, and the intravenous infusion rate was adjusted to 100 ml/h by intravenous flow control line. Therefore, the bradycardia due to the drug event was excluded. Because intraoperative ETCO2 was 34–37 mmHg and SpO2 was 97–100%, airway or ventilation problem were also excluded. Since there was no direct stimulation of vagus nerve or mechanical compression of the carotid sinus, direct vagal stimulation or baroreceptor reflex was excluded. It is reasonable to diagnose bradycardia due to TCR because sudden severe bradycardia occurred during surgical stimulation of trigeminal nerve territory and heart rate was restored as soon as surgical stimulation was stopped.
The term TCR was first reported in 1988 by Shelly and Church [9]. However, the definition of TCR remains unclear, as strict criteria for TCR have not yet been determined. Only clinical manifestations have been reported, such as sudden severe bradycardia, asystole, arterial hypotension, and transient cardiac arrest during stimulation of the territory of the trigeminal nerve [3,10]. In this case, there was severe bradycardia without arterial hypotension. We thought arterial hypotension has occurred, but was not detected becauseintermittent NIBP monitoring was performed.
Stimulation of trigeminal branches or nerve endings triggers afferent signals to the Gasserian ganglion. This stimulation activates the sensory nucleus of the trigeminal nerve in the fourth ventricle floor. Small internuncial nerve fibers of the reticular formation connect premotor neurons in the nucleus ambiguus and the dorsal motor nucleus of the vagus nerve. A reflex pathway activates cardioinhibitory parasympathetic vagal neurons to complete the reflex arc (Fig. 2) [3,6,7].
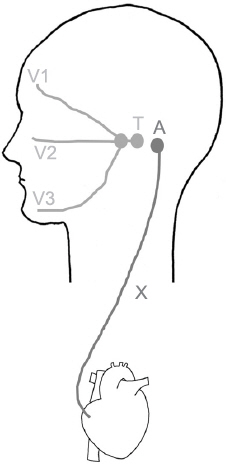
Trigeminocardiac reflex pathway. Stimulation of trigeminal branches triggers afferent signals to the Gasserian ganglion. This stimulation activates the trigeminal nucleus. Small internuncial nerve fibers connect premotor neurons in the nucleus ambiguus and the dorsal motor nucleus of the vagus nerve. V1: ophthalmic branch, V2: maxillary branch, V3: mandibular branch, T: trigeminal nucleus, A: nucleus ambiguus, X: vagus nerve.
The TCR is subdivided into a central TCR and a peripheral TCR based on the stimulated site. The peripheral TCR is subtyped into the OCR and the maxillomandibulocardiac reflex, based on the division of the stimulated trigeminal nerve [3,10].
Cambell et al. [11] reported cases of cardiac arrest and bradycardia associated with maxillectomy in 1994. There have been at least 60 reported deaths due to TCR during maxillofacial surgery [1,6]. However, the TCR is rarely reported in the context of surgery of the mandibular branch of the trigeminal nerve. The risk of TCR always must be considered in cases of surgery in the territory of the trigeminal nerve. Risk factors for TCR constitute light general anesthesia, younger age (owing to higher resting vagal tone), hypoxemia, hypercarbia, and long-lasting provoking stimulus. Accordingly, these factors should be corrected prior to the performance of craniofacial surgery. Mechanical traction is the most potent predisposing factor to stimulation of the TCR [3,7].
In the present case, during surgery, there was no hypoxemia (SpO2 100%), hypercarbia (ETCO2 33–35 mmHg), or light general anesthesia (BIS was maintained at 40–50). However, there was strong traction of the wire in the right mandibular angle. It is thought that the strong traction induced stimulation of the mandibular branch of the trigeminal nerve, with subsequent activation of the TCR.
Termination or minimization of manipulation is recommended as the first treatment. If bradycardia and hypotension do not respond to the interruption of surgery, intravenous anticholinergics (atropine or glycopyrrolate) should be administered [1,3,7]. Epinephrine may be effective in patients who do not respond to anticholinergics [3,10]. In the present case, atropine injection was required during the first occurrence of TCR. However, upon the second TCR attack, the heart rate returned to 70 beats/min as soon as the traction was terminated, without pharmaceutical intervention.
While there have been several reports of refractory TCR requiring immediate cardiac life support, this phenomenon seems rare. TCR may produce very poor outcomes [4,12]. However, with careful monitoring and immediate management, these events could be resolved in most cases.
In conclusion, because of the possibility of severe bradycardia, asystole, or cardiac arrest when induced, it is important to be aware of the possible occurrence of TCR during manipulation of division III of the trigeminal nerve, especially during surgical stimulation of the TMJ.
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
ORCID
Yeojung Kim: https://orcid.org/0000-0002-2079-670X
Boohwi Hong: https://orcid.org/0000-0003-2468-9271
Yongsup Shin: https://orcid.org/0000-0001-5071-734X
Chan Noh: https://orcid.org/0000-0003-4904-148X
Seounghun Lee: https://orcid.org/0000-0002-6424-2477
Seokhwan Hong: https://orcid.org/0000-0002-5362-1893
