Nerve blocks for optimal postoperative analgesia after total knee arthroplasty
Article information
Abstract
The use of ideal pain management modalities after total knee arthroplasty facilitates enhanced recovery by promoting early ambulation and controlling postoperative pain. To achieve these goals, multimodal analgesia, including motor-sparing peripheral nerve blocks, appears to be promising in older adults undergoing total knee arthroplasty. This review describes optimal nerve blocks, as a part of multimodal analgesia for total knee arthroplasty, and the scientific basis of each technique.
INTRODUCTION
Total knee arthroplasty (TKA) is a common surgical procedure for treating patients experiencing chronic pain associated with advanced osteoarthritis. TKA, however, is a painful procedure, and inadequate postoperative analgesia hinders rehabilitation, prolongs hospitalization, and is associated with an increased risk for adverse events including myocardial ischemia, pulmonary dysfunction, and thromboembolism. There are multiple strategies to control postoperative pain after TKA, including administration of systemic or intrathecal opioids, local infiltration of analgesia, and peripheral nerve blocks (PNBs). The ideal pain management modality should provide excellent analgesia while minimizing opioid consumption and enhancing rehabilitation [1–3]. Given the prospect of improved postoperative pain control and reduced opioid consumption, multimodal analgesia, including PNBs, appears to be promising in older adults undergoing TKA. The purpose of this review is to describe optimal analgesic blocks, as a part of multimodal analgesia used for TKA, and the scientific basis of each block.
NERVOUS INNERVATION OF THE KNEE
The knee joint is primarily innervated by the femoral, obturator, and sciatic nerves. Branches of the femoral nerve to the knee are primarily the saphenous nerve, intermediate and medial femoral cutaneous nerves and, additionally, nerves to the vastus lateralis, intermedius, and medialis muscles. The most common approach to TKA is the medial parapatellar arthrotomy, which involves a longitudinal midline incision through the skin and subcutaneous tissue extending from 5 cm proximal to the superior pole of the patella to the tibial tuberosity. A medial parapatellar arthrotomy, through the anteromedial aspect of the skin, subcutaneous tissue, deep fascia, retinacular ligaments, and fibrous capsule, will evoke pain mediated mainly by the infrapatellar branch of the saphenous nerve, the terminal branch of the nerve to the vastus medialis muscle, and the anterior branch of the medial femoral cutaneous nerve [3,4]. Intra-articular innervations of the menisci, perimeniscular joint capsule, cruciate ligaments, infrapatellar fat pad, and posterior part of the fibrous knee capsule are supplied by the tibial nerve and posterior branch of the obturator nerve [4].
SPECIFIC PERIPHERAL NERVE BLOCKS
PNBs not only reduce pain but also have a positive effect on resource use after TKA. PNBs for TKA have been reported to be associated with decreased length of hospital stay and a significant reduction in the risk for readmission [5]. In a recent network meta-analysis, which ranked the efficacy of 17 available analgesic modalities, five combinations that were most effective for pain at rest included femoral/obturator, femoral/ sciatic/obturator, lumbar plexus/sciatic, femoral/sciatic, and fascia iliaca compartment blocks. In addition, the five most effective combinations for reduction of opioid consumption are the femoral/sciatic/obturator, femoral/obturator, lumbar plexus/sciatic, lumbar plexus, and femoral/sciatic blocks [1]. Considering all aspects, the combination of femoral and sciatic nerve block was considered the gold-standard PNB for patients undergoing TKA in this meta-analysis [1]. In another meta-analysis, sciatic nerve block in combination with femoral nerve block was reported to significantly reduce postoperative opioid consumption and knee pain following TKA compared with femoral nerve block alone [6]. Although providing superior analgesia, femoral and sciatic nerve blocks have not been widely integrated in the setting of fast-track pathways or enhanced recovery after surgery protocols at ambulatory joint replacement centers due to concerns for associated motor weakness and delayed ambulation [7,8]. Recently, some studies have described motor-sparing PNBs and alternative periarticular injections, which may enhance patient recovery by promoting early ambulation and reducing postoperative pain [7,9–11]. In addition, continuous PNB is suggested as an alternative analgesic modality, which consists of a percutaneously inserted catheter with its tip adjacent to a target nerve and the administration of local anesthetic, providing a prolonged block [12–14].
Femoral nerve block
Clinical background and anatomy
Branches of the femoral nerve innervate the anteromedial part of the knee, which pass through the femoral triangle and adductor canal. The femoral neurovascular bundle descends under the sartorius muscle into the groove of the femoral triangle at the apex of the iliopectineal fossa. The saphenous nerve, femoral artery, and femoral vein exit the femoral triangle at the apex and enter the adductor canal. Proximally in the femoral triangle, motor branches, which supply the rectus femoris muscle and the vastus muscles, emerge. Thus, femoral nerve block administered at this level can decrease the strength of the quadriceps muscle and increase the risk for falls [15]. Distally in the femoral triangle, subsartorial injection anterolateral to the femoral artery blocks the saphenous nerve, the nerve to the vastus medialis muscle, and medial femoral cutaneous nerve.
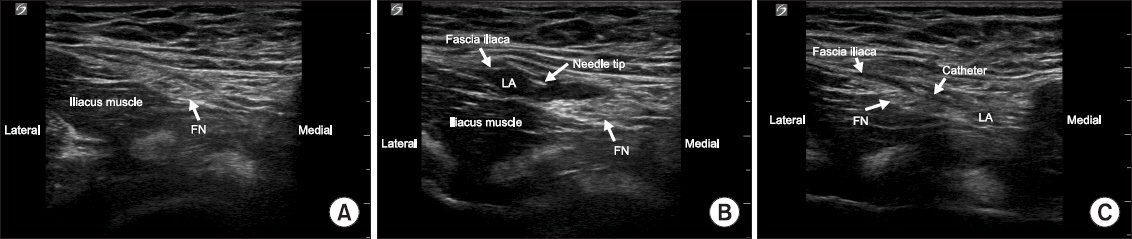
Ultrasound-guided block techniques
With the patient supine, the transducer is applied transversely to the femoral crease to identify the femoral nerve by slightly tilting the transducer cranially or caudally. After examination of the anatomy of the femoral artery and nerve, the nerve is targeted at a level immediately above the bifurcation of the deep femoral artery (Fig. 1A). The needle is inserted inplane from lateral to medial, and advanced towards the lateral aspect of the femoral nerve below the fascia iliaca. Proper deposition of local anesthetic is confirmed either by observation of the femoral nerve being displaced by the injection or by the spread of the local anesthetic above or below the femoral nerve (Fig. 1B). Circumferential deposit of local anesth etic around the femoral nerve confers no clinical advantage for this block [16]. A pool of local anesthetic adjacent to either the posterolateral or anterior aspect of the femoral nerve is sufficient. If continuous femoral nerve block is indicated, an 18-gauge Tuohy needle is inserted in-plane from the anterolateral side of the transducer though the fascia iliaca. After local anesthetic distribution is ensured, a 20-gauge perineural catheter is subsequently inserted 2–3 cm past the needle tip (Fig. 1C). Finally, the needle is withdrawn over the catheter, which is fixed in place with a sterile clear adhesive dressing and then connected to an infusion pump programmed for ropivacaine 0.2% infusion after surgery.
Adductor canal block
Clinical background and anatomy
The adductor canal begins at the apex of the femoral triangle and ends at the adductor hiatus. It is bordered anteriorly by the sartorius muscle, laterally by the vastus medialis muscle, and posteromedially by the adductor longus/magnus muscles (Fig. 2). This triangular inter-muscular tunnel lies posterior to the sartorius muscle and is a passageway for the major neurovascular bundle of the thigh from the femoral triangle to popliteal fossa. In a recent anatomical study, both the saphenous nerve and nerve to the vastus medialis were consistently identified along the adductor canal, whereas branches of the anterior obturator nerve were inconsistently present [17]. The saphenous nerve contributes to innervation of the knee capsule through superficial infrapatellar and posterior branches, as well as to the origin of the deep genicular nerves. The nerve to vastus medialis contributes to innervation of the knee capsule through the intramuscular, extramuscular, and deep genicular nerves. Enhanced early mobilization after TKA has recently increased interest in the search for more peripheral sites at which to administer local anesthesia to preserve the strength of the quadriceps muscle postoperatively [18]. In a recent meta-analysis, adductor canal block demonstrated better preservation of strength of the quadriceps muscle and improved mobilization ability, resulting in better functional recovery after TKA without compromising pain control compared with femoral nerve block [19].
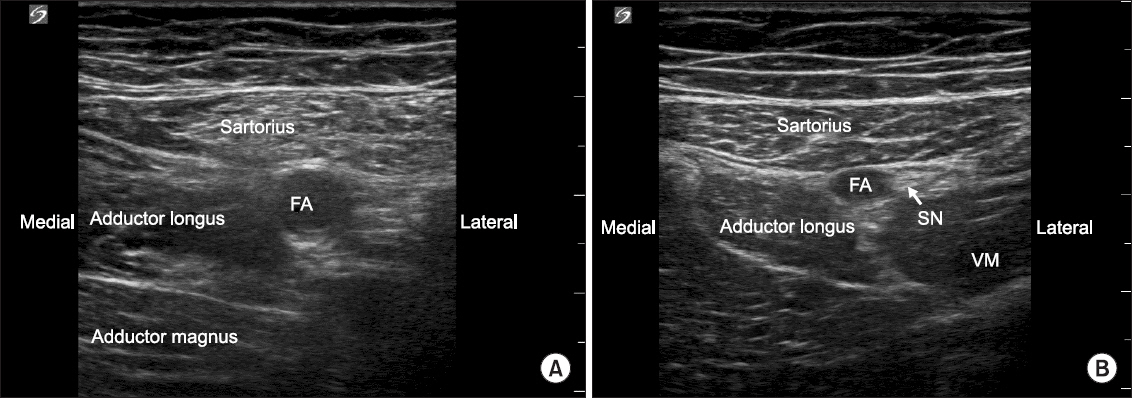
Ultrasound images of the short-axis view of halfway between the anterior superior iliac spine and base of the patella (A) and proximal end of the adductor canal (B). FA: femoral artery, SN: saphenous nerve, VM: vastus medialis.
Recent anatomical studies have reported some issues surrounding subsartorial femoral triangle block and true adductor canal block [3,17,20,21]. The true adductor canal begins at the site where the medial border of the sartorius muscle crosses over the medial border of the adductor longus muscle and could be located more distally than the midpoint of the thigh (halfway between the anterior superior iliac spine and base of the patella) [17]. Although the two terms are used interchangeably, recent studies reporting the efficacy of adductor canal block for TKA actually performed ultrasound-guided block at mid-thigh level [7,12,18,22,23].
Ultrasound-guided block techniques
An ultrasound transducer is placed in the transverse cross-sectional position to obtain the short-axis view of the adductor canal and its contents. The femoral artery is identified beneath the sartorius muscle with the vein immediately underneath the artery and the saphenous nerve immediately lateral to it. The saphenous nerve usually appears in the midthigh region lateral to the artery as a hyperechoic structure. The needle is inserted in-plane from the lateral to medial aspect and advanced toward the femoral artery, through the sartorius muscle, with the tip of the needle placed lateral to the artery under the vastoadductor membrane. Local anesthetic is injected to spread lateral to the femoral artery and deep to the sartorius muscle, or more distal, below the knee.
Continuous adductor canal blocks provide postoperative analgesia after surgical procedures involving the knee [12–14]. If continuous adductor canal block is indicated, an 18-gauge Tuohy needle is inserted in-plane from the anterolateral side of the transducer through the sartorius muscle with the needle tip positioned between the femoral artery and the saphenous nerve. After local anesthetic is injected, a 20-gauge perineural catheter is inserted 2–3 cm beyond the tip of the Tuohy needle. The most commonly used local anesthetic regimen is ropivacaine 0.2% infusion via the perineural catheter at a basal rate of 6–10 ml/h for 24–48 h after surgery.
Obturator nerve block
Clinical background and anatomy
The obturator nerve enters the thigh through the obturator canal and immediately divides into an anterior and a posterior branch. This posterior branch descends between the adductor brevis and magnus muscles and pierces the adductor magnus muscle. It then descends along the posterior surface of the adductor magnus muscle and joins branches from the tibial nerve in the popliteal plexus, which innervate the intraarticular structures of the knee joint [3]. In some instances, when the posterior branch is absent, a distal branch from the anterior branch of the obturator nerve contributes to the popliteal plexus [3].
Ultrasound-guided block techniques
The transducer is advanced medially along the femoral crease to identify the pectineus and adductor muscles. The obturator nerve can be blocked using an ultrasound-guided subpectineal approach in the interfascial plane between the pectineus and external obturator muscles (Fig. 3A). Slightly distal to the inguinal crease on the medial aspect of the thigh, the anterior and posterior branches of the obturator nerve can be selectively blocked in the interfascial space between the adductor brevis and longus muscles and in the subinguinal region between the adductor brevis and magnus muscles, respectively (Fig. 3B). A block needle is advanced in-plane from the lateral to medial aspect and into the interfascial space between the muscles.
Infiltration between the popliteal artery and the capsule of the knee (IPACK) block
Clinical background and anatomy
The smaller branches of the tibial part of the sciatic nerve, 10–25 cm proximal to the genicular joint line, form the popliteal plexus together with the posterior branch of obturator nerve. While a popliteal sciatic nerve block is not expected to cover the tibial genicular nerve branch to the popliteal plexus, transgluteal and subgluteal approaches may result in a compromised ability to ambulate. Recent studies have described selective blockade of the popliteal plexus as a perivascular approach or infiltration between the popliteal vessels and posterior knee capsule to block genicular contribution from the obturator and tibial nerves [7,8]. IPACK block provides analgesia to the posterior capsule of the knee joint without compromising foot strength or affecting the medial and lateral superior genicular nerves [24,25].
Ultrasound-guided block techniques
IPACK block anesthetizes articular branches on the posterior aspect of the knee, which may be performed at the popliteal fossa above the patella. At the level where the femoral condyles merge with the shaft of the femur, tibial and peroneal nerves are visualized superficial to the popliteal artery, and the leg is positioned with the knee flexed and hip externally rotated (Fig. 4). After identifying the space between the femur and popliteal artery, the needle is advanced in-plane from the medial to lateral aspect toward the lateral border near the periosteum of the femur. Infiltration of local anesthetic is performed incrementally in the area between the artery and femur, finishing at the medial end of the femur.
CONCLUSION
Femoral and sciatic nerve blocks may be considered the “gold standard” and provide superior analgesia after TKA. However, profound muscle weakness associated with the combination of these blocks prohibits fast-track protocols after TKA. Therefore, subsartorial femoral triangle block or adductor canal block (midway between the anterior superior iliac spine and base of the patella) may be ideal for enhanced recovery after surgery by providing effective analgesia and improving the ability to ambulate after medial parapatellar arthrotomy. In addition, supplemental blockade of the popliteal plexus using an obturator nerve block or local anesthetic infiltration of the posterior genicular capsule or IPACK block would reduce postoperative pain and improve ambulation.
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
ORCID
Bora Lee: https://orcid.org/0000-0002-7699-967X