INTRODUCTION
In shoulder surgery, arthroscopic procedures are popular and widely used because they enable a smaller incision, less tissue injury, a wider surgical field, less postoperative pain and potentially faster recovery [
1,
2]. To achieve successful surgery with an arthroscope, a mechanical fluid-irrigation system (irrigation pump, as below) is used to produce adequate joints distension and wash out blood and cell debris from the joint space [
3].
Although, an irrigation pump can efficiently provide a clear surgical vision, if used with extra-ordinary high pressure or for longer periods than expected, it can cause a number of deleterious side effects, including compartment syndrome, synovial pouch rupture, and fluid extravasation [
4,
5]. Among them, fluid extravasation is an uncommon side effect in arthroscopic shoulder surgery using an irrigation-pump system, but fluid can be extended through the carotid space and consequently can cause an airway obstruction after surgery, which can be a fatal complication. A number of studies have reported this side effect [
6-
8]. To prevent extravasation, an irrigation pump should be maintained at as low a pressure as possible, which can be achieved by a proper block of surgical stimulus and bleeding at the articular space.
Desflurane can allow fast induction and emergence from anesthesia [
9]. However, some studies have reported that desflurane can increase sympathetic nerve activity, and plasma catecholamine release more than other inhalation anesthetic agents [
10,
11]. High level of plasma catecholamine is associated with increased blood flow in several tissues and stimulates fibrinolytic activity [
12-
16]. Therefore, during arthroscopic surgery, desflurane may theoretically cause more bleeding in articular spaces and may need a higher irrigation-pump pressure to achieve clear vision in the surgical site than with other inhalation agents.
We hypothesized that desflurane could cause an increase in the required irrigation pump pressure compared to sevoflurane during shoulder surgery under arthroscopy. Thus, the objective of this study was to test this hypothesis.
MATERIALS AND METHODS
This study was a single-center, prospective, randomized, double-blind clinical trial. The study protocol was approved by our Institutional Review Board (no. NHIMC 2018-02-007). Written informed consent was obtained from all patients. Patients undergoing elective, unilateral rotator cuff repair surgery under general anesthesia without brachial plexus nerve block were eligible for participation. All patients were under age 75 with American Society of Anesthesiologist classification I-II. Exclusion criteria were uncontrolled hypertension, a history of myocardial infarction, cerebral ischemia, cerebral hemorrhage and acute or chronic renal failure and abnormal blood coagulation profile (prothrombin time, activated partial thromboplastin time and platelet count) at preoperative test. Patients were randomized via concealed enveloped method into two groups, sevoflurane group (group S) or desflurane group (group D). Each group had 20 patients.
In the operating room, all patients were monitored by means of electrocardiography, non-invasive blood pressure, pulse oximetry, and a bispectral index (BIS) electrode on the forehead and baseline data were recorded. Before induction of anesthesia, patients breathed 100% O2 for two minutes. Anesthesia was induced with 1.5 mg/kg intravenous propofol and continuous infusion of remifentanil (Ultian, Hanrim, Korea) at 3 ng/ml on effector-site mode with a target-controlled infusion system (TCI, Base Primea, Fresenius Kabi, Germany). After loss of consciousness, patients were ventilated manually using a face mask 1.2 MAC either with sevoflurane (SojournŌäó, Piramal critical care, USA) or desflurane (Suprane, Baxter, USA) in 100% O2. A dose of 0.6 mg/kg rocuronium was used to facilitate endotracheal intubation. Anesthesia was maintained with FiO2 0.4 mixed with medical air with total flow 2 L/min and sevoflurane or desflurane. Ventilation was controlled using an anesthesia machine (Aisys, Datex-ohmeda, USA) to maintain end-tidal CO2 (EtCO2) level between 35-40 mmHg. Remifentanil was infused by a TCI pump to keep the BIS value below 40 during the whole period of operation and the total amount was recorded.
Patients were positioned laterally with the shoulder to be operated on exposed on top. For group S patients, sevoflurane 1.2 MAC (end-tidal concentration 2.0-2.2 vol%) and intravenous remifentanil with TCI were administered for anesthesia maintenance. For group D patients, desflurane 1.2 MAC (end-tidal concentration 7.0-7.4 vol%) and intravenous remifentanil with TCI were administered. No other methods were used to reduce blood pressure for improvement of surgical site visibility. In the event of hypotension (< 80 mmHg in systolic blood pressure) or in marked bradycardia (< 45 beats per minute), intravenous ephedrine 4-12 mg was injected.
A shoulder arthroscope connected to a water pump inflow tube was inserted at the glenohumeral joint. Then the mechanical irrigation-pump (Synergy
®, Arthrex, Germany) was started at 20 mmHg pressure to inflate the joint space with 0.9% saline solution. The surgeon then estimated the visibility of the surgical field (Grade I: excellent, Grade II: good, Grade III: reasonable, Grade IV: poor) [
16,
17]. Subsequently, the pressure was freely adjusted by the surgeon to obtain clear vision with the arthroscope during the surgery. The attending anesthesiologist recorded the maximum pressure used during the operation. The same surgeon performed every operation without knowing the patientsŌĆÖ assignment.
The primary end point of this study was to find the maximum pressure of the water pump needed to achieve the clearest vision of the surgical site during the entire operation. The second set of end points were surgical field visibility at the beginning of surgery and the systolic and diastolic blood pressure and heart rate at start of surgery, and 20, 40, and 60 min after that. We also collected surgical time, amount of infused remifentanil, and the use of ephedrine.
A sample size collection was calculated by a pilot study. Ten patients were enrolled, and five randomly assigned to each group. Anesthetic induction and maintenance were conducted with the above parameters and methods. The primary end point, maximum water-pump pressure, was collected. For group S patients, mean and standard deviation of the pressure was 40.0 ┬▒ 10.0 mmHg. For group D patients, it was 54.0 ┬▒ 9.0 mmHg. Thus, we calculated the sample size as a total of 40 (20 per group) at significance level of 0.01, and power of 90% including the assumption of 20% drop-out rate.
All data were analyzed with SPSS 21.0 software package for Windows (IBM Co., USA). Demographic data in continuous form, the maximum pressure of the water pump, surgical time and the total dosage of remifentanil were analyzed by an independent t-test. Systolic and diastolic pressure and the pulse rate in each period were analyzed by repeated measures ANOVA with the Bonferroni correction after normality test. And after sphericity testing, we used Greenhouse-Geisser test. Other nominal variables (arthroscopic visibility, ephedrine use) were analyzed by chi-square test or FisherŌĆÖs exact test. A P < 0.01 was considered statistically significant.
RESULTS
One patient in group S was excluded because the scheduled arthroscopic repair of a torn rotator cuff had changed into open repair with autonomous ligament transplantation. No patient complained with symptoms of airway obstruction after the operation.
There were no significant differences between the groups in demographic data, total amount of remifentanil dose, surgical time or ephedrine use between the two groups (
Table 1).
Table┬Ā1
|
Variables |
Group S (n = 19) |
Group D (n = 20) |
P value |
|
Sex (M/F) |
7/12 |
9/11 |
0.113 |
|
Age (yr) |
62.3 ┬▒ 8.4 |
62.5 ┬▒ 6.7 |
0.956 |
|
Height (cm) |
159.3 ┬▒ 7.8 |
162.5 ┬▒ 9.8 |
0.271 |
|
Weight (kg) |
63.4 ┬▒ 11.7 |
64.9 ┬▒ 7.7 |
0.641 |
|
Prothrombin time (s) |
10.8 ┬▒ 0.5 |
10.7 ┬▒ 0.6 |
0.412 |
|
Activated partial thromboplastin time (s) |
24.5 ┬▒ 2.2 |
25.2 ┬▒ 3.1 |
0.420 |
|
Platelet count (├Ś103/┬Ąl) |
222.4 ┬▒ 48.2 |
249.1 ┬▒ 75.9 |
0.201 |
|
Remifentanil dose (┬Ąg) |
686.6 ┬▒ 284.4 |
631.8 ┬▒ 274.7 |
0.544 |
|
Surgical time (min) |
115.0 ┬▒ 28.3 |
95.8 ┬▒ 32.8 |
0.058 |
|
Ephedrine use |
4 |
3 |
0.695 |
The maximum pressure of the mechanical water pump was higher in group D than group S (54.0 ┬▒ 6.8 mmHg vs. 48.9 ┬▒ 5.7 mmHg, P = 0.017,
Table 2), but the difference was not statistically significant at a significance level of 0.01. Furthermore, the arthroscopic visibility at the start of surgery did not differ significantly between the two groups (P = 0.284,
Table 2).
Table┬Ā2
Visibility and Pressure of Water Pump
|
|
Group S (n = 19) |
Group D (n = 20) |
P value |
|
Arthroscopic visibility |
|
Grade I/II/III/IV |
10/5/4/0 |
5/7/7/1 |
0.284 |
|
Maximum pressure of irrigation pump (mmHg) |
48.9 ┬▒ 5.7 |
54.0 ┬▒ 6.8 |
0.017 |
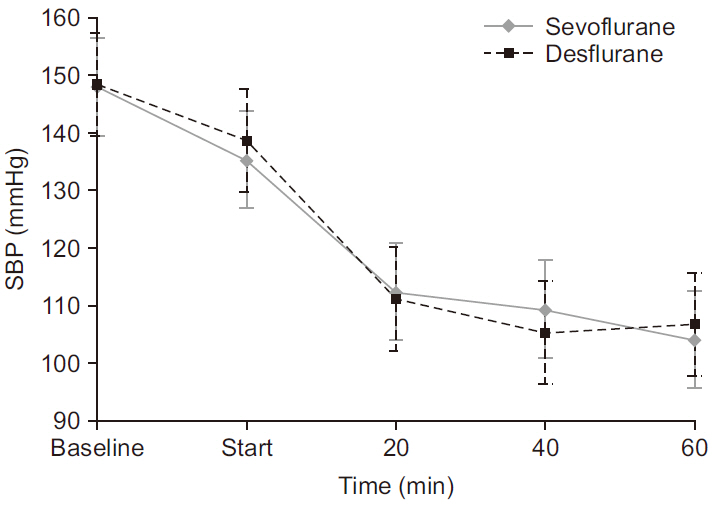
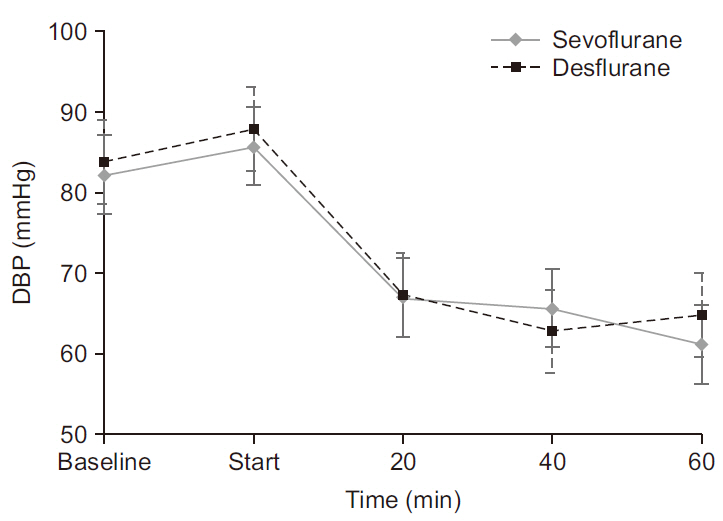
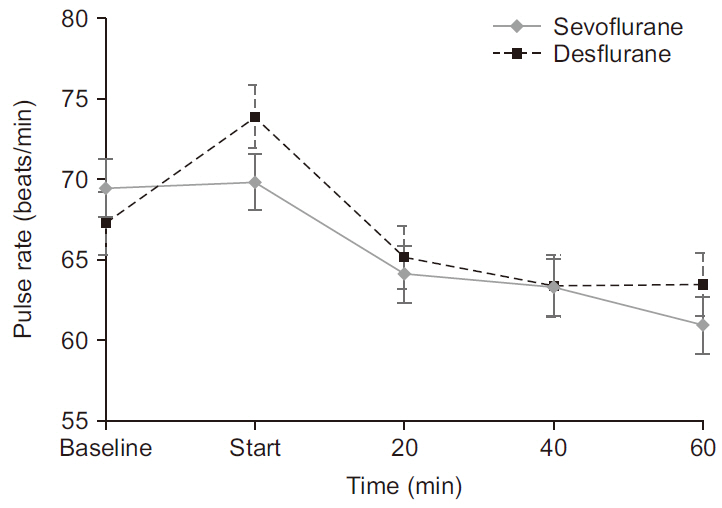
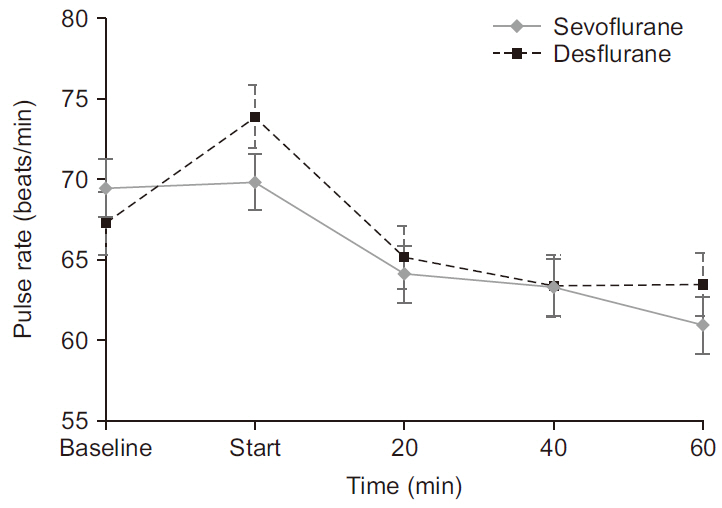
Systolic blood pressure, diastolic blood pressure and pulse rate in both groups showed a decrease over time (P < 0.001). However, these parameters were not significantly different between the two groups (P = 0.955, P = 0.709, P = 0.682, respectively,
Fig. 1-
3).
Fig.┬Ā1
Systolic blood pressure (SBP) at time schedule. Baseline, surgical start, 20, 40, and 60 min after surgical start. Values are presented as means ┬▒ SD. There were no differences between two groups in systolic pressure (P = 0.955).
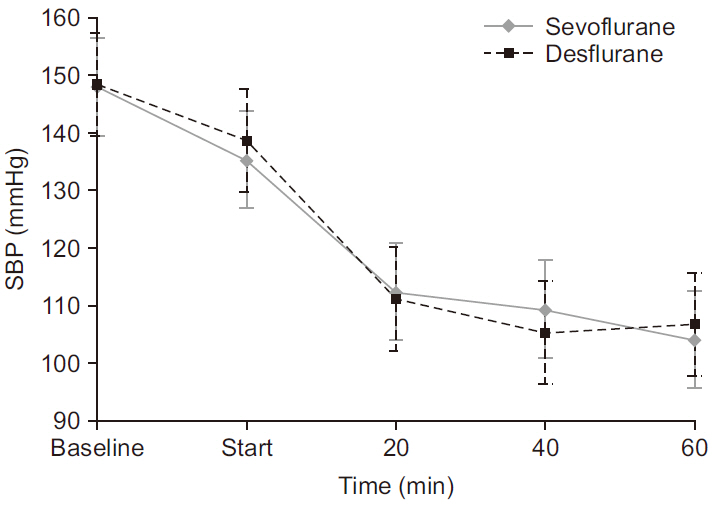
Fig.┬Ā2
Diastolic blood pressure (DBP) at time schedule. Baseline, surgical start, 20, 40, and 60 min after surgical start. Values are presented as means ┬▒ SD. There were no differences between two groups in diastolic pressure (P = 0.709).
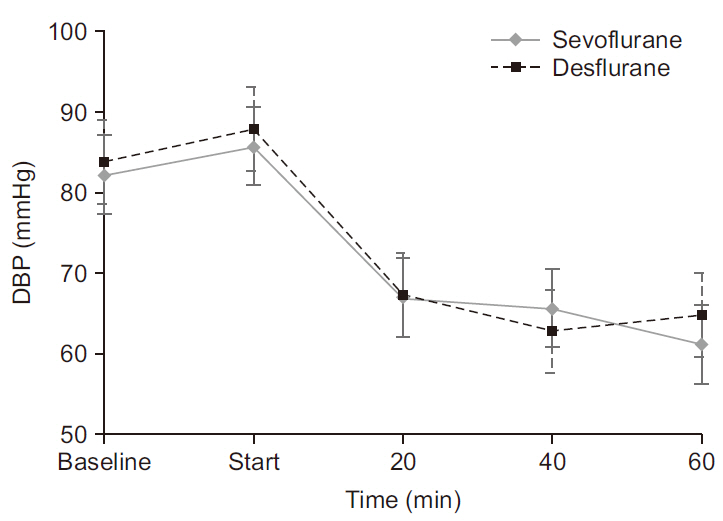
Fig.┬Ā3
Pulse rate at time schedule. Baseline, surgical start, 20, 40, 60 min after surgical start. Values are presented as means ┬▒ SD. There were no differences between two groups in pulse rate (P = 0.682). At the start of surgery, pulse rate of desflurane group was slightly higher than sevoflurane group. But, statistically, there were no differences between groups in pulse rate (P = 0.682).
DISCUSSION
In this study, the maximum irrigation pump pressure in shoulder arthroscopy was not different between the two groups. The desflurane group on average needed higher pressure than the sevoflurane group, but it was not different statistically (P = 0.017).
In the literature, there are studies which have focused on the neuroendocrine effects of surgery with desflurane. Marana et al. [
11], reported that plasma adrenaline and noradrenaline concentrations were higher in desflurane treated patients than those that received sevoflurane during and immediately after laparoscopic pelvic surgery. They found that compared to sevoflurane, the desflurane group showed higher serum adrenaline and noradrenaline 30 min after the start of surgery and 30 min following completion of surgery. Leung and Pastor [
10], compared the effects of desflurane and isoflurane on plasma catecholamine level in patients undergoing major non-cardiac surgery. They also showed that plasma norepinephrine level was higher in the desflurane group, 1, 5, and 10 min after tracheal intubation and plasma epinephrine level was statistically higher 1 min after tracheal intubation in the desflurane group than the isoflurane group.
High levels of plasma epinephrine are associated with increased blood flow due to reduced vascular resistance in several tissues and increased fibrinolytic activity. Bading et al. [
12], reported that epidural anesthesia with epinephrine infusion was associated with a 3.5-fold reduction in calf vascular resistance and an increase in calf blood flow of 170%. By contrast, epidural anesthesia with norepinephrine was associated with no change in calf vascular resistance but, a 1.4-fold reduction in calf blood flow. They concluded that ╬▓ adrenergic activity was responsive in the skeletal muscle even after cardiac ╬▓ receptors were down-regulated in the elderly.
Another study reported that epinephrine can attenuate the activation of coagulation and increase activation of the fibrinolytic system [
14,
15]. Based on these studies, it seems reasonable to assume that desflurane compared to other inhalation anesthetics would produce more blood flow and fibrinolytic activity in surgical fields because of elevated plasma epinephrine level.
Therefore, we hypothesized that patients anesthetized with desflurane in arthroscopic shoulder surgery, would have increased muscular blood flow and fibrinolytic stimulation due to sympathetic nerve system activation, especially epinephrine. Thus, it might cause more bleeding in the articular system. Consequently, greater pressure from the irrigation pump might be needed to clarify the cloudy fluid in the articular space. However, we failed to uncover any difference in irrigating pump pressure between the desflurane group and the sevoflurane group.
Several possible explanation for our findings suggest themselves; first, according to prior studies, epinephrine would produce an increase in blood flow and fibrinolytic activity via ╬▓ adrenergic receptors but norepinephrine would not. Unfortunately, we did not evaluate serum catecholamine level, but we think that co-elevated norepinephrine and other ╬▒-agonists would interrupt the effects of epinephrine. Second, the concurrently used remifentanil could block the hemodynamic effects of elevated catecholamine caused by desflurane. According to Leung and Pastor [
10], despite higher plasma catecholamine levels after tracheal intubation, hemodynamic data such as heart rate, systolic blood pressure and left ventricular ejection fraction were not statistically different between desflurane group and isoflurane group. They concluded that hemodynamic instability could be modulated by concurrently used opioids and beta blockade [
10]. Likewise, in our study, higher plasma catecholamine in desflurane group would increase blood pressure and heart rate to a greater degree than sevoflurane group, which might cause more bleeding in shoulder articular space. However, hemodynamic data during the surgery and the arthroscopic visibility at surgical start did not differ between the two groups. We presumed that remifentanil would have blocked these hemodynamic instabilities.
Shoulder arthroscopy became a major diagnostic tool and therapeutic option for many shoulder disorders. Despite the fact it is a the minimally invasive technique, the rate of complications ranges from 2 to 5%, including nerve palsy, local infection, and arthritis, articular cartilage damage, rotator cuff tear, and extraarticular fluid leakage [
4,
6-
8].
Among these, the extraarticular leakage of fluid, commonly into the deltoid muscle and chest cavity, is a well-recognized complication [
18], although typically it is a clinically insignificant symptom and is reabsorbed within 12 h [
6]. Sometimes however, a significant amount of fluid can extend through the carotid space to the paratracheal space resulting in critical airway obstruction. Several articles have reported this life-threatening complication [
6-
8]. The risk factors for this complication are increased joint irrigating-pump pressure, obesity, duration of the arthroscopic procedure, and arthroscopy within the subacromial space, because this space is not closed within the capsule [
7]. However, the critical value for irrigating pressure and length of surgery, remain unclear.
This study has limitations. First, we did not measure plasma catecholamine level during surgery and compare between the two groups. Second, hopefully, if we could quantitate the degree of accumulation of free water around the trachea or carotid space after surgery, we could figure out the risk of the arthroscopic shoulder surgery directly.
In conclusion, patients anesthetized with desflurane in arthroscopic shoulder surgery do not need greater irrigating fluid pump pressure than those anesthetized with sevoflurane in order to secure a clear vision of the surgical site.
ACKNOWLEDGMENTS
This work was supported by National Health Insurance Service Ilsan Hospital grant NHIMC2018CR007.
REFERENCES
Br├╝lhart KB, Roggo A, Kossmann T, Duff C, Schimmer R, Glinz W. 1993 Arthroscopy of the shoulder joint. Technique, indications, surgery and complications. Langenbecks Arch Chir 378: 200-5. German. PMID:
10.1007/BF00184361. PMID:
8366732.

Yamaguchi K, Levine WN, Marra G, Galatz LM, Klepps S, Flatow EL. 2003; Transitioning to arthroscopic rotator cuff repair: the pros and cons. Instr Course Lect 52: 81-92. PMID:
10.2106/00004623-200301000-00022. PMID:
12690842.


Hsiao MS, Kusnezov N, Sieg RN, Owens BD, Herzog JP. 2016; Use of an irrigation pump system in arthroscopic procedures. Orthopedics 39: e474-8. PMID:
10.3928/01477447-20160427-01. PMID:
27135450.


Moen TC, Rudolph GH, Caswell K, Espinoza C, Burkhead WZ Jr, Krishnan SG. 2014; Complications of shoulder arthroscopy. J Am Acad Orthop Surg 22: 410-9. PMID:
10.5435/JAAOS-22-07-410. PMID:
24966247.


Bomberg BC, Hurley PE, Clark CA, McLaughlin CS. 1992; Complications associated with the use of an infusion pump during knee arthroscopy. Arthroscopy 8: 224-8. PMID:
10.1016/0749-8063(92)90040-I. PMID:
1637436.


Borgeat A, Bird P, Ekatodramis G, Dumont C. 2000; Tracheal compression caused by periarticular fluid accumulation: a rare complication of shoulder surgery. J Shoulder Elbow Surg 9: 443-5. PMID:
10.1067/mse.2000.109320. PMID:
11075331.


Saeki N, Kawamoto M. 2011; Tracheal obstruction caused by fluid extravasation during shoulder arthroscopy. Anaesth Intensive Care 39: 317-8. PMID:
21485693.

Leung JM, Pastor DA. 1998; Dissociation between haemodynamics and sympathetic activation during anaesthetic induction with desfluranes. Can J Anaesth 45: 533-40. PMID:
10.1007/BF03012703. PMID:
9669006.



Marana E, Russo A, Colicci S, Polidori L, Bevilacqua F, Viviani D, et al. 2013; Desflurane versus sevoflurane: a comparison on stress response. Minerva Anestesiol 79: 7-14. PMID:
23090102.

Bading B, Blank SG, Sculco TP, Pickering TG, Sharrock NE. 1994; Augmentation of calf blood flow by epinephrine infusion during lumbar epidural anesthesia. Anesth Analg 78: 1119-24. PMID:
10.1213/00000539-199406000-00015. PMID:
8198268.


Freyschuss U, Hjemdahl P, Juhlin-Dannfelt A, Linde B. 1986; Cardiovascular and metabolic responses to low dose adrenaline infusion: an invasive study in humans. Clin Sci (Lond) 70: 199-206. PMID:
10.1042/cs0700199. PMID:
3956110.



van der Poll T T, Levi M, Dentener M, Jansen PM, Coyle SM, Braxton CC, et al. 1997; Epinephrine exerts anticoagulant effects during human endotoxemia. J Exp Med 185: 1143-8. PMID:
10.1084/jem.185.6.1143. PMID:
9091588. PMID:
PMC2196238.




Ostrowski SR, Henriksen HH, Stensballe J, Gybel-Brask M, Cardenas JC, Baer LA, et al. 2017; Sympathoadrenal activation and endotheliopathy are drivers of hypocoagulability and hyperfibrinolysis in trauma: A prospective observational study of 404 severely injured patients. J Trauma Acute Care Surg 82: 293-301. PMID:
10.1097/TA.0000000000001304. PMID:
27779595.


Zini C, Stieven-Filho E, Tabushi FI, Ribas CA, Ribas FM, Opolski AC, et al. 2016; Knee arthroscopic visibility alterations in obese and non-obese patients. Arq Bras Cir Dig 29(Suppl 1): 75-9. PMID:
10.1590/0102-6720201600s10019. PMID:
27683782. PMID:
PMC5064278.



Johnson DS, Stewart H, Hirst P, Harper NJ. 2000; Is tourniquet use necessary for knee arthroscopy? Arthroscopy 16: 648-51. PMID:
10.1053/jars.2000.4826. PMID:
10976127.