INTRODUCTION
In December 2014, the Act for the Improvement of Patient Safety and Medical Quality was established in Korea. Subsequently, the debate surrounding medical disputes continues to be one of the most controversial issues. Moreover, the rapid advancements in medical technology have increased the likelihood of medical disputes due to the variety of medical practices available [
1,
2]. This trend is particularly noticeable within the field of pain management. The nature of pain management is characterized by a subjective difference in the perception of pain, and it is dependent on individual differences in physiological, emotional, and cognitive states [
3]. Furthermore, the likelihood of the occurrence of adverse events, including complications, is gradually increasing. This is due to pain physicians having diverse training backgrounds, increases in the utilization of interventional pain procedures (ranging from nerve blocks to minimally invasive surgery), and increases in the use of various analgesics, including opioids, each with different mechanisms.
The Act for the Relief of Medical Accidents and Adjustment of Medical Disputes in Korea defines a “medical accident” as a case in which a person’s life, body, and/or property are damaged by diagnosis, examination, treatment, and/or prescription or preparation of medications. Therefore, not all medical accidents indicate a medical error. Even if there was no medical error, medical disputes can occur if a patient makes a claim [
4]. In some cases, such medical disputes may lead to medical litigation. With this trend, great economic and emotional burdens are brought to both patients and physicians, resulting in an increase in defensive medicine [
5].
Recently, medical dispute cases have risen annually due to the significant changes in people’s ability to acquire information and knowledge. Additionally, the increased use of invasive procedures, an increase in specialized hospitals related to pain management, and an aging society are predicted to lead to further increases in medical disputes and lawsuits related to treatment. Domestic institutions have focused on the resolution of medical disputes and are still seeking a fundamental solution to prevent medical accidents. Understanding the situations in which complications leading to lawsuits may arise is most important for pain physicians. However, there are few published studies presenting data on medical-dispute cases related to pain management in Korea.
Korea Medical Dispute Mediation and Arbitration Agency (KMDA), which is a public institution under the Ministry of Health and Welfare, was established in 2012 to support the redemption of damages caused by medical accidents by resolving medical disputes quickly and fairly in Korea.
The aim of this study was to analyze the judicial precedent of pain management cases from KMDA to assess the specific details of the incidents, the economic burden, and how the settlement of damages and liabilities was resolved in Korea.
DISCUSSION
In Korea, there is no official or consistent statistical information regarding the number of medical disputes; therefore, accurate predictions are limited [
9]. Nonetheless, the number of arbitration cases over medical disputes filed in Korea has been steadily increasing [
10,
11]. Despite the growing likelihood of medical accidents, it has been highlighted that there is a lack of system to report medical accidents and it is challenging to accurately identify the status of medical accidents.
In this study, we analyzed cases of disputes related to pain treatment that were referred to the KMDA for the first time between 2012 and 2016. Our results suggest that medical disputes occur for various reasons with cases of different parts of the body being affected in clinical practice in pain management. When classifying according to medical specialty, dispute cases were often reported in the departments of orthopedic surgery, anesthesia, and pain medicine. Moreover, oriental medicine was involved in several cases, which reflects the cultural preference for oriental medicine in Korea compared with other countries.
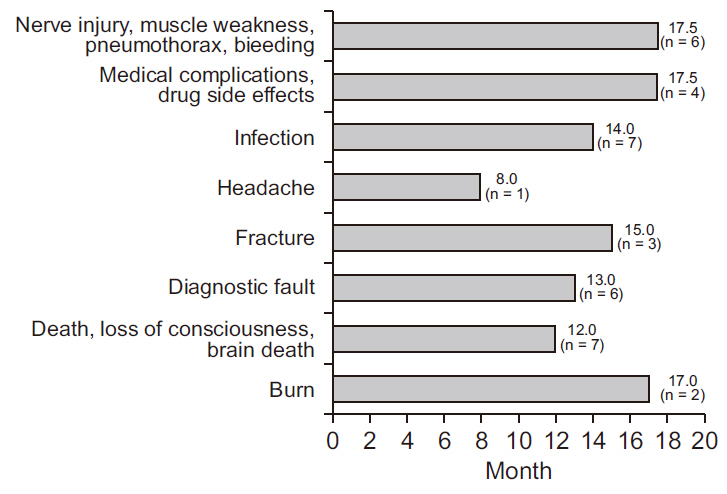
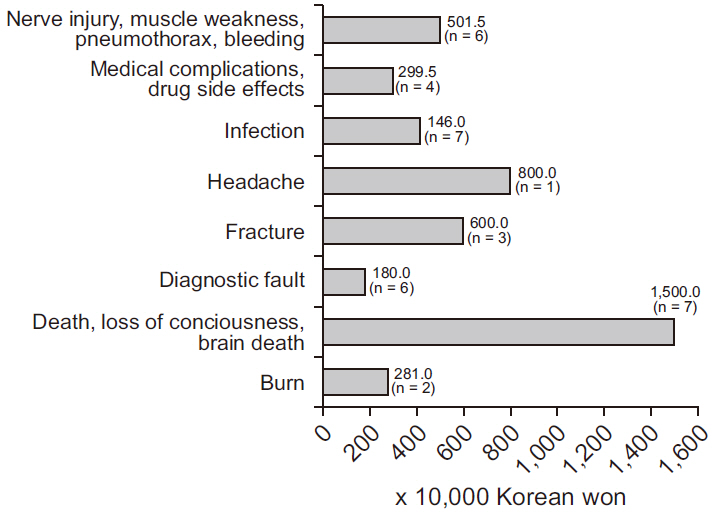
The median time taken from the time of the event to reaching an agreement was 17.7 months. However, it was difficult to generalize as the content varies and the number of cases is limited. We observed that it took longer to reach an agreement following outcomes such as nerve damage, muscle weakness, and diagnosis than in cases of death, fracture, and among others. This is probably because the outcomes of medical practice take longer to occur than the treatment or confirmation of a diagnosis if there are many side effects. The time taken to resolve a conflict can place a huge burden on both patients and physicians. Moreover, the social costs can also have negative effects, increasing the need for efforts to prevent similar medical accidents.
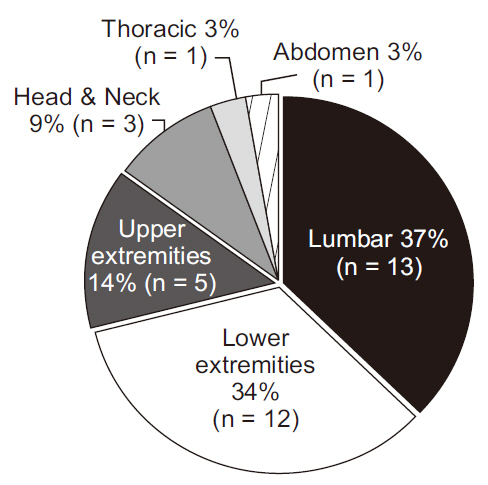
The anatomical location that contributed most to conflicts was the lumbar region (37% of cases). This result is consistent with those of previous studies reporting a high prevalence of cases involving the musculoskeletal system [
12,
13]. Although it is possible to expect improvement in symptoms of back pain with conservative therapy, the likelihood of treatment with interventional methods is increasing. This increase likely results from an aging population, as well as an increase in the number of treatment options and consumer expectations due to advancements in medical technology [
14].
The lack of accurate information about the management of spinal pain and evidence-based approaches of new techniques may also play a role [
15]. The involvement of the upper and lower extremities and the shoulder was also similar to the results of other studies, but the involvement of the knee was less commonly reported [
6].
A previous study has reported the analysis of 630 cases of domestic medical disputes from 2000 to 2007 [
16]. In this study, medical practice that was recognized to be negligent was reported in 115 cases (31.9%) with surgery or other procedures.
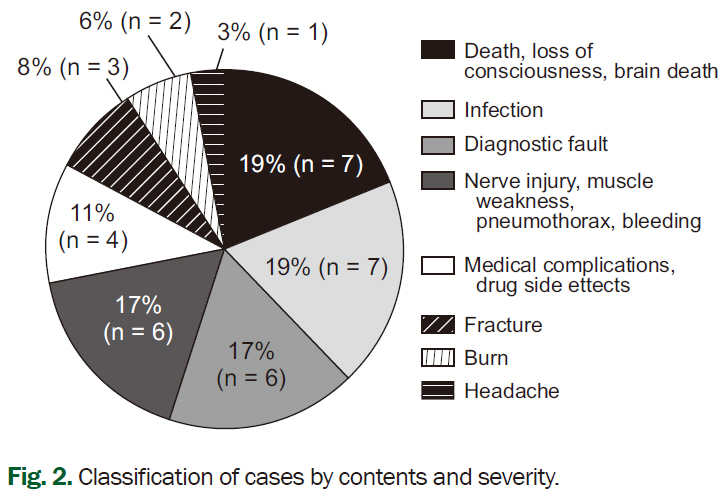
Meanwhile, it was reported in 73 cases (20.3%) regarding diagnosis, 63 cases (17.5%) regarding patient monitoring, and 26 cases (7.2%) regarding patient transfer. In comparison, in our study, focusing pain treatment, most dispute cases were related to injection therapy including nerve block, which can be considered within surgery and other procedures (n = 14, 38%). In a study analyzing medico-legal malpractice claims in the United States, similar results to ours were reported [
17], with nerve injury (23%), pneumothorax (21%), and infection (13%) being the most common cases. Nonetheless, there were also considerable numbers of cases involving non-invasive medical practices, such as diagnostic concerns and adverse reactions to medication (n = 10, 28%).
A previous study on medication management in pain management reviewed cases in the United States and reported an increasing number of claims from 2 to 8% of total cases a year from 1977 to 2004 [
18]. There was a trend for claims focused on opioids to be from younger patients with back pain. A history of depression, obtaining medications from multiple providers, and a history of alcohol abuse were also considered to be major contributors. However, no cases of conflict involving drug-related opioids have yet been observed in our results.
Medical accidents can occur unexpectedly in medical practice and do not necessarily indicate a medical error. As medical practice entails certain risks, culture and system that treats medical accidents as value-neutral and encourages systematic reporting and analysis of medical accidents are necessary.
We also reviewed points of the dispute in each case and identified several issues, which are often debated in the course of a lawsuit. Causal relationships, medical malpractice, and duty of informed consent were the issues that have been mainly discussed. Lawsuits associated with a lack of informed consent would not happen if there a written consent with adequate explanation. Otherwise, it carries a potentially devastating toll of cost and disruption to a physician’s practice. The process of informed consent is a complex inter-relationship among the patient, physician, and society. The ultimate goal of informed consent is a well-informed and educated patient who understands their individual conditions during pain management. Obtaining true informed consent that will withstand judicial scrutiny is well worth the effort. As taking the time to ensure effective patient communication and establishing documentation to ensure effective informed consent will not only benefit the physician/patient relationship, it will also help insulate the physician from costly liability claims. Medical validity should also be reconsidered when using an evidence-based approach. Cost-effectiveness, as well as therapeutic effects, has to be considered during the process of detailed informed consent. Pain management is extremely complex, and adverse events are an occasional eventuality even with the most cautious practice. However, if the patient is clearly aware of inherent risks and accepts these by choosing to proceed with either a procedure or a treatment plan, the physician has performed a duty in the patient’s best interest.
Although there was a study on the medico-legal dispute related to pain management in Korea [
6], Medical dispute cases related to pain management still have not been well reviewed due to limited information available. This is the first study focused on legal responsibility, actual mutual compensation amount, and time spent which were never reviewed.
For limitations, as analyzed using judgment data, it was not possible to identify any information that was anonymized to protect personal information. Medical accidents in medical litigation decisions as analyzed in this study cannot be generalized to medical accidents occurring within medical institutions, and it is possible that they differ from actual cases occurring frequently. In addition, the arbitration panel’s judgment process focuses on which processes caused the mistake, as they often judge only the claims made by the plaintiff or defendant and not by the medical practitioner.
However, despite these limitations, we analyzed the results of recent medical dispute settlements related to pain management, which enabled an assessment of the status of legal disputes for pain treatment in Korea.
We suggest that system data should be organized based on the findings of our study. The development of various diagnostic techniques and the application of new drug therapies have the potential to increase relevant cases in future in Korea. Efforts are ongoing to plan ahead systematically. In particular, guidelines and recommendations for pain management are needed, especially those focused on medico-legal cases.