Necrotizing fasciitis likely mistaken for chronic low back pain - A case report -
Article information
Abstract
Necrotizing fasciitis is a significant factor of morbidity and mortality due to its sudden onset and rapid spread. It is accompanied by systemic toxicity and often fatal unless promptly recognized and aggressively treated. We reported a patient who presented symptoms confused with disc herniation and delayed initial diagnosis. The patient was treated for chronic low back pain. The origin of the pain was a foreign body-induced intra-abdominal infection that invaded the back muscles and eventually progressed to necrotizing fasciitis.
Necrotizing fasciitis is one of the fatal soft-tissue infections reported with a mortality rate ranging from 6% to 76%. The symptoms are very diverse and can be alleviated by early invasive surgical removal. In the early stages, it may be difficult to diagnose because the symptoms present only as pain at the site without evidence of infection. Therefore, patients who have been treated with chronic pain at the same site may develop a differential diagnosis after disease progression. Although the etiology of the disease is varied, as in our case, infectious agents in the intra-abdominal cavity are rarely reported to form fistulas with subcutaneous tissue. We report a case of delayed immediate diagnosis of necrotizing fasciitis in a patient with chronic low back pain.
CASE REPORT
A 68-year-old man had received medical treatment for low back pain for 1 year. One week before admission, he received outpatient care of aggravated right buttock and low back pain. At that time, he had to reserve magnetic resonance imaging (MRI) for a more accurate diagnosis. Then, he underwent caudal block at a nearby hospital 3 day before admission. However, the symptoms did not improve during the weekend but worsened, and hospitalized treatment was planned. On admission, he complained of right iliac area pain and a tingling sensation on the right leg. He reported that the pain continued to deteriorate and was localized, but no other neurological symptoms were observed. In addition, there was no aggravation or relief factor of these symptoms. The vital signs were as follows: heart rate, 114 beats/min; noninvasive blood pressure (BP), 90/60 mmHg; and body temperature, 36.6°C. Lumbar spine MRI showed L4–5 level disc herniation with right soft-tissue mass, which invaded the iliacus muscle (Fig. 1). On the first day of hospitalization, the patient underwent abdominal and pelvic precontrast computed tomography for differential diagnosis with a suspicion of abscess due to a high fever of 40.1°C with localized heat and tenderness in the right flank area (Fig. 2). The laboratory findings were as follows: white blood cells (WBC), 28,700/μl; segmented neutrophil, 89.8%; erythrocyte sedimentation rate, 86 mm/h; C-reactive protein (CRP), 27.61 mg/dl; and procalcitonin, 1.55 ng/ml. The mean BP was maintained above 60 mmHg by continuous infusion of norepinephrine at 32 mcg/min.
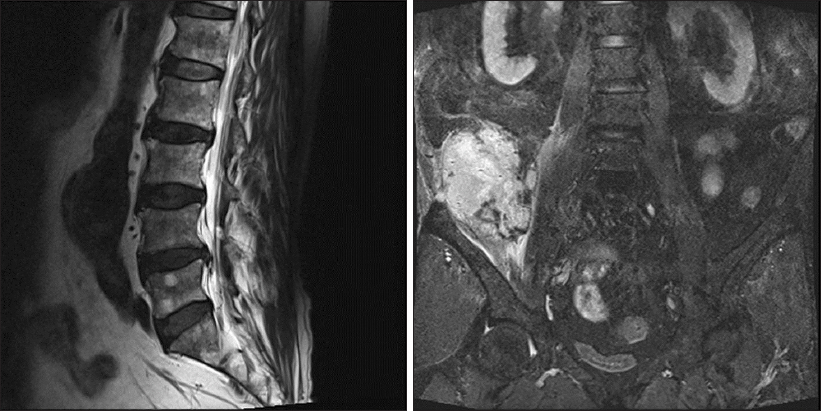
Lumbar spine magnetic resonance imaging showing central to left paracentral disc protrusion at L4–5 with annular tear disc bulge at L3–4 and L2–3. In addition, there is soft-tissue intensity in the right pre-iliac lesion measuring 10.0 × 3.0 × 5.0 cm suggesting a parailiac phlegmon involving the right iliacus muscle.
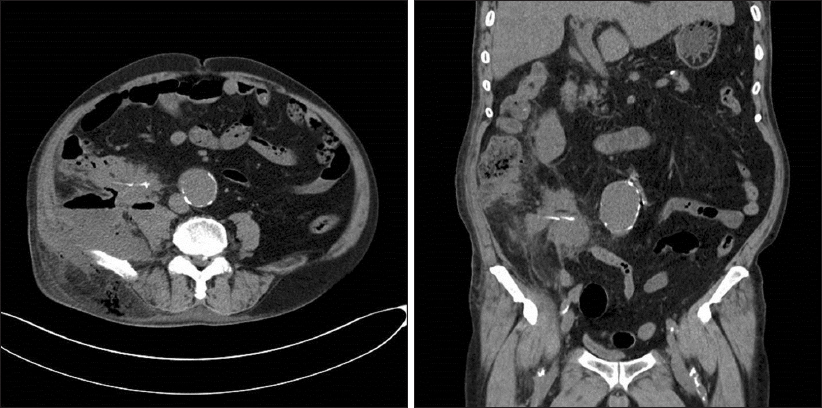
Precontrast computed tomography showing soft-tissue lesion (10.5 cm) in the right posterior pararenal space, psoas muscle, iliacus muscle, and right posterior abdominal wall. A linear high-density lesion is seen adjacent to the terminal ileum.
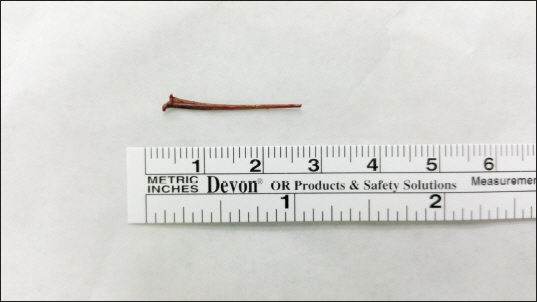
The first debridement was performed under local anesthesia in the right flank area, and intensive care was started according to septic shock regimen. A huge abscess pocket on the right buttock extended to the right lower abdomen. Then, explorative laparotomy was performed under general anesthesia for debridement of all infected tissues in the abdominal cavity. Surgical findings showed an abscess pocket extending from the posterior distal ileum to the cecum and a 2.5 cm fish bone in the infected tissue (Fig. 3). After the operation, the patient underwent an additional interview about past history. He had no abdominal discomfort or fever, but had three to four diarrhea episodes 1 week before admission. The patient reported that he had not eaten raw fish, but did eat boiled fish soup.
After the main surgery, laboratory findings were improved as WBC, 15,500/μl; segmented neutrophil, 74.4%; and CRP, 11.27 mg/dl. Moreover, the patient maintained a stable vital sign without any infusion of inotropes. Several additional debridement and antibiotics continued, and he was transferred to the general ward at 3 weeks of hospitalization. He was discharged 2 months after admission. He is currently undergoing follow-up in the outpatient department in relation to the underlying disease.
DISCUSSION
Necrotizing soft-tissue infections (NSTIs) can occur in any area of the body but is most commonly seen in the extremities, perineum, and genitalia, with fewer cases arising on the chest or abdomen [1]. Early signs and symptoms are identical to those seen in cellulitis or abscesses, potentially making the correct diagnosis difficult. Patients who present with signs and symptoms of systemic toxicity or shock already have very advanced disease. Treatment consists of radical debridement, broad-spectrum antimicrobial therapy, and hemodynamic support. Delayed time to proper management is associated with increased mortality [2–5]. Therefore, early diagnosis and surgical debridement have repeatedly been shown to improve outcomes [6–8].
The most adopted scoring method is the laboratory risk indication for necrotizing fasciitis (LRINEC) developed by Wong et al. [9]. LRINEC is a method of scoring several test results, such as CRP, WBC, hemoglobin, and serum levels of sodium, creatinine, and glucose. According to this method, the patient had 4 points for CRP, 2 points for WBC and creatinine, 1 point for hemoglobin, 0 for sodium and glucose levels, with a total score of 9 points. Our patient’s LRINEC score was 9 points, with high category probability of NSTI > 75% at admission. However, when the patient first visited the outpatient clinic, there were no suspicious symptoms of infection, such as fever, heat sensations, or unstable vital signs, and the patient’s symptoms did not differ from the previous case of disc herniation [10]. Therefore, the possibility of an intra-abdominal infection was overlooked. It is very unusual for such a foreign body to induce intraperitoneal infection leading to persistent inflammation and fistula tract. The present case required close coordination between surgical and critical care teams.
An external origin (e.g., injection site, insect bite, boils, etc.) would present with erythema, vesicles, and crepitus at the infected area. In addition, the physical examination shows definite tenderness of the area. If the tenderness in the abdomen or the costovertebral angle was checked during physical examination, it may have been possible to detect the abnormal symptoms earlier [11,12]. In the end, detailed history taking and accurate physical examinations can be more meaningful than any test results.
Our patient had persistent low back pain for 1 year and received delayed proper initial management until the onset of the recent symptoms indicated an infection. Such extensive soft-tissue infections have vague symptoms, with sudden onset and rapid spread. Therefore, early diagnosis and aggressive treatment are important. If the patient’s neurologic symptoms do not indicate a significant difference compared with the extent of pain; given that pain is localized over time and tenderness becomes prominent, we need to consider differential diagnosis of other causes. Furthermore, when the pain pattern is unclear or localized tenderness is absent, intra-abdominal infection should be ruled out by testing for evidence of peritoneal irritation, such as prominent rebound tenderness or exacerbation with coughing.
ACKNOWLEDGMENTS
We thank the intensive care unit staff and primary care physicians for their help and management for this patient.