Repeated endotracheal tube cuff tears during nasotracheal intubation due to nasal cavity orthodontic micro-implant - A case report -
Article information
Abstract
Background
Nasotracheal intubation is generally performed for intraoral surgery.
Case
A 34-year-old female patient who underwent orthognathic surgery exhibited repeated endotracheal tube cuff tears during nasotracheal intubation. After intubation, leaks developed, and torn endotracheal cuff was observed in the removed endotracheal tube. Subsequently, re-intubation through the same nasal cavity was performed immediately, but leakage from the torn endotracheal tube cuff was re-observed. A leakage test of the extubated tube revealed air bubbles and leaks near the tube cuff due to the tear. Nasotracheal intubation was performed through the other nasal cavity, and there were no leakage findings or abnormalities. During the course of the surgery, the surgeon noticed that the orthodontic micro-implant deposited in the mid-tube cavity was exposed to the nasal cavity.
Conclusions
We aimed to emphasize caution and discuss the possibility that orthodontic micro-implants that are not confirmed during preoperative evaluation may cause repeated endotracheal tube cuff tears.
Tracheal intubation is essential for maintaining the airway during general anesthesia. When performing endotracheal intubation, air leakage is one of the most common complications. The lack of ventilation caused by endotracheal tube cuff tears accounts for 5.9% to 11% of air leakage complications [1,2]. A damaged cuff can lead to a variety of complications, ranging from minor issues, such as air bubbles in the oral cavity, to fatal respiratory complications. Since immediate reintubation may entail risks associated with hypoxia and airway maintenance failure, damage to the endotracheal tube cuff during endotracheal intubation is an important issue that requires caution [3].
For orthognathic surgery, nasotracheal intubation, namely endotracheal intubation through the nasal cavity, is usually performed. Among patients who undergo orthognathic surgery, the skeletal anchorage system (SAS) is implemented in some patients for orthodontic correction. The micro-screws used for orthodontic correction are also called SAS screws, orthodontic anchoring screws, mini-screws, and micro-implants [4]. In this case, they are referred to as orthodontic micro-implants. Micro-implants placed in the middle of the palate can play the role of indenting the molar teeth or tilting the molar to the buccal side [4].
In this report, we present the first case of repetitive endotracheal tube cuff damage caused by orthodontic micro-implants during nasotracheal intubation.
CASE REPORT
Institutional Review Board waived the requirement of written consent for the publication of this case (no. CAUH-2101-016-19352).
A 34-year-old female patient (height, 168 cm; weight, 59 kg) was scheduled to undergo orthognathic surgery under general anesthesia for malocclusion and facial asymmetry. The patient had no medical history or specific findings other than orthodontic findings. Preoperative imaging examinations were performed, including facial and intraoral surface anatomy photography, panoramic X-ray photography, and cone-beam computed tomography, which showed no specific findings in either the nasal or nasopharyngeal regions (Fig. 1). Pulse oximetry, noninvasive blood pressure monitoring, and electrocardiography monitoring were initiated after the patient entered the operating room. Before the induction of anesthesia, her blood pressure was 110/70 mmHg, heart rate was 70 beats per minute, and pulse oxygen saturation was 99%.
Before the induction of anesthesia, the nasal tube (Nasal RAE, COVIDIENTM, Ireland) with an inner diameter of 6.5 mm was assessed preoperatively for any leakages on the cuff by immersing the tube of the endotracheal tube in a 1-L bottle of normal saline solution. Approximately 10 ml of air was injected into the cuff, but no air bubbles were observed. The anterior part of the endotracheal tube was also immersed in normal saline solution at 37°C for 5 min to soften the nasal tube.
For the induction of anesthesia, 100 μg of fentanyl, 40 mg of 2% lidocaine, 120 mg of 1% propofol, and 40 mg of rocuronium were administered after sufficient oxygenation through 100% oxygen. Nasotracheal intubation was performed via the right nasal cavity. In passing the tube through the nasal cavity, the anesthesiologist perceived slight stiffness without bleeding or other difficulties. After passage through the nasal cavity, a laryngoscope and Magill forceps were used for tracheal intubation. Due to the risk of rupture of the cuff, the anesthesiologist intended not to handle the cuff of the nasotracheal tube using the Magill forceps. Tracheal intubation was performed without any particular difficulty (Cormack–Lehane grade I). After nasotracheal intubation, clear symmetric breathing sounds were heard in both lungs, and the cuff did not leak immediately after injecting air into the cuff. Ten minutes after mechanical ventilation, positive pressure ventilation was applied, and the gap between the inspiratory volume and expiratory volume began to increase. There was leakage of anesthetic gas into the oral cavity, and a leakage sound was heard in the oral cavity. Re-intubation was attempted under the suspicion of cuff rupture. A nasotracheal tube with an inner diameter of 6.0 mm, which was one size smaller than the size of the previous tube, was assessed again for tube leakage and re-intubated through the right nasal cavity.
In the process of passing through the nasal cavity, as in the first attempt, the anesthesiologist perceived slight stiffness, and the tube was assessed using a laryngoscope and intubated into the vocal cords without using Magill forceps. However, immediately after intubation, a cuff tear was observed, and the tracheal tube was removed. The anesthesiologist repositioned the tube from the right to the left nasal cavity, and a nasal tube with an internal diameter of 6.0 mm was reinserted. Unlike on the right side, the nasotracheal tube passed through the left nasal cavity smoothly without any perception of stiffness. After air injection, no findings of air leakage in the endotracheal tube were observed, both lung auscultations were symmetric and clear, no sounds from the outflow of oral auscultation were heard, and the tidal volume was properly obtained through positive mechanical ventilation. Subsequently, the surgery proceeded well without any leakage, and maintenance of anesthesia was performed using 50% nitrous oxide and oxygen mixed fresh gas and 6–7 vol% desflurane.
During the dental surgery, the micro-implant screw, which was fixed at a position 3 mm from the central line to the right from the single-stage ceiling, was found by the surgeon (Fig. 2). On incision of the maxilla, the surgeon confirmed that the tip had protruded approximately 1–2 mm in the nasal cavity. The cause of the cuff tear of the nasotracheal tube during repeated intubation via the right nasal trachea was finally confirmed. Subsequently, the surgery was completed without any complications.
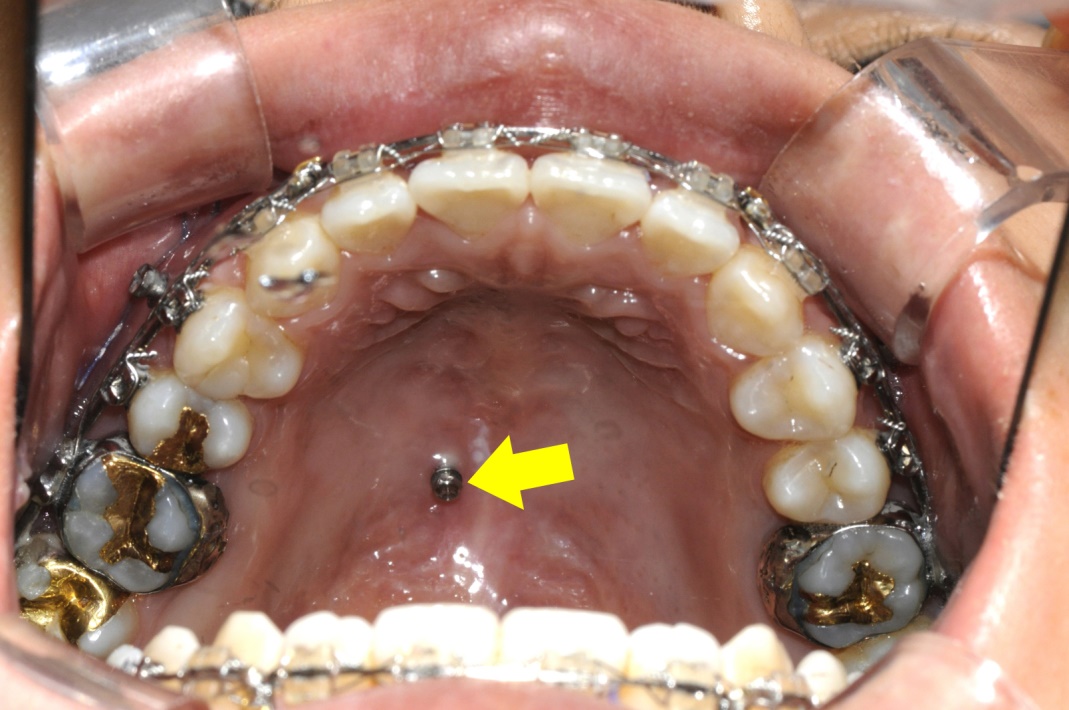
Image of the micro-implant protruding from the single-stage ceiling in the patient. The micro-implant screw was fixed at a position 3 mm from the central line to the right from the single-stage ceiling. Tip of yellow arrow represent the micro-implant screw.
The screw, which was an orthodontic micro-implant, is used for dental orthodontics. Since the micro-implant was inserted between the imaging test and surgery, we did not detect the position of the micro-implant before the surgery. Radiography and computed tomography performed on the 1st day after the surgery revealed findings leading to the suspicion of orthodontic micro-implants (Figs. 3, 4).
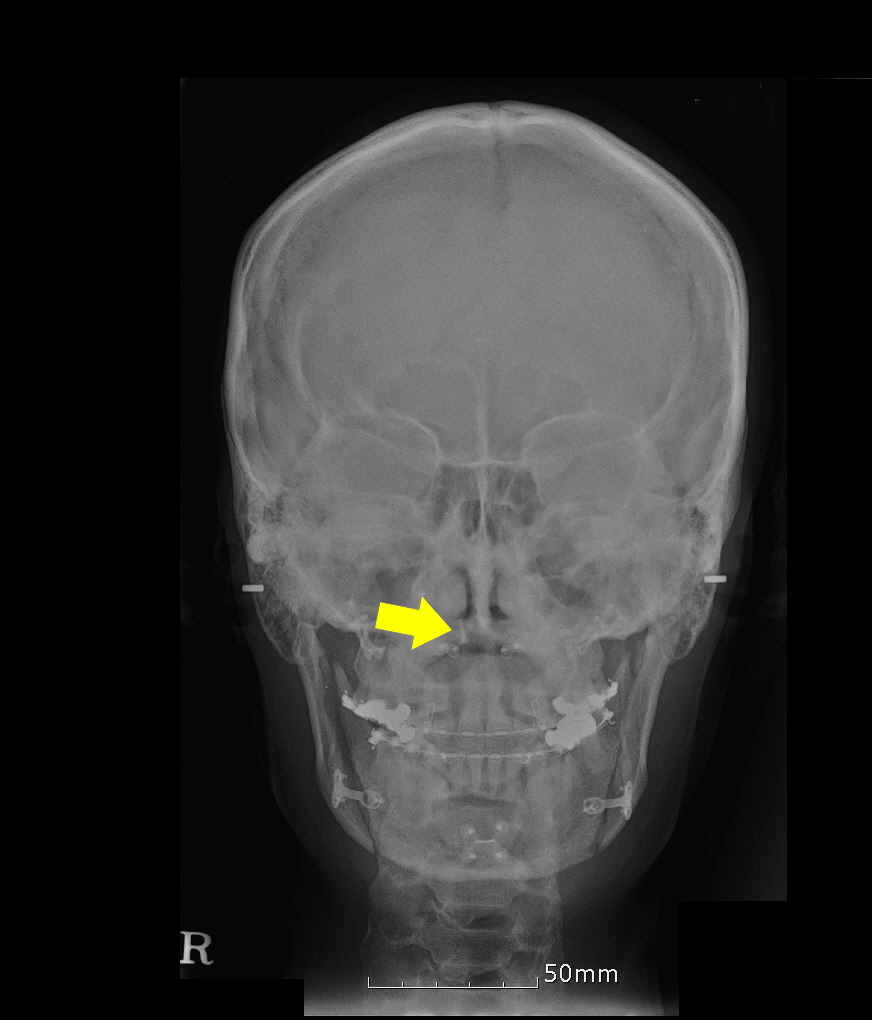
Postoperative skull radiography. Postoperative skull radiography showed a screw protruding into the right nasal cavity, which was not observed on preoperative radiography. Tip of yellow arrow represent the micro-implant screw.
DISCUSSION
Nasotracheal intubation is generally performed when the oral route cannot be used in patients who have undergone head and neck, oral, or open impairment surgery. It is also performed as an alternative to tracheostomy when long-term intubation maintenance is required in the intensive care unit [5,6]. In particular, nasotracheal intubation facilitates securing a surgical field of view in orthognathic surgery. However, nasotracheal intubation is associated with a higher risk of cuff damage because the passage of the nasal cavity is narrow and there are more structures compared to the oral cavity. Abnormal structures that can affect nasotracheal intubation include concha bullosa, septal curvature, septal spurs, nasal polyps, and other anatomical variations [7]. Therefore, intubation is performed by using a route that contains fewer abnormal structures that may affect nasotracheal intubation. This is because nasotracheal intubation may not be successful in cases of a narrow nasal cavity, and abnormal structures may damage the tube cuff. In addition, cuff tears may occur because of the Magill forceps used for intubation through the nasal cavity. Therefore, an anesthesiologist must take care not to handle the tube cuff when intubating via the vocal cords and trachea in the oropharynx [8,9].
The nasal cavity is divided into two sides by the nasal wall. The lower wall is composed of the oral cavity and hard palate, and the upper wall is composed of the middle wall of the maxillary sinus and three nasal bones. When performing nasotracheal intubation, the nasal tube passes through the nasal canal via two routes: the upper and lower routes [10]. In the upper route, the tube passes through the space between the middle turbinate and inferior turbinate, and in the lower route, it passes through the space between the bottom of the nasal cavity and inferior turbinate [11]. The lower route is known to be safer because it does not pass near the middle turbinate, which is rich in vascular structures [4,12]. In our case, we suggest that the right nasotracheal intubation had entered through the lower route of the nasal canal both times, and the intubation was perceived as slightly stiff as it passed through a narrow space. In this case, the anesthesiologist detected the rupture and leakage of the cuff and performed reintubation. In the second trial, a tube that was one size smaller was used, and in the third trial, the intubation was repositioned from the right to the left to prevent respiratory complications related to hypoxia.
In some cases, orthognathic surgery may be performed with a micro-implant inserted for further correction. In this situation, there is the possibility of a nasotracheal tube cuff tear by the micro-implant. Micro-implants, which are usually used for orthodontics, are 1.2 mm in diameter and have a screw 6–8 mm in length. In our case, a micro-implant with a diameter of 1.4 mm and length of 6 mm was inserted in the part that had deviated to the right by 3 to 3.5 mm from the middle of the upper palate. The location of micro-implants varies, but it is possible in most of the areas with alveolar bone of the maxilla or mandible, as well as alveolar bones such as the buccal or labial bone, palatal alveolar bone, maxillary nodule of maxilla, mid-maxillary palatal bone, posterior teeth, and body part of the maxilla [13,14]. Micro-implants placed in the middle of the palate in this way can play a role in indenting the molar teeth or tilting the molar to the buccal side [4].
Although the intranasal screw does not protrude after normal orthodontic treatment, there may be some complications following micro-implant placement, such as inflammation, infection, root contact, fractures, and swelling [13]. Therefore, additional orthodontic treatment should be avoided after preoperative imaging tests. We suggest that it is necessary to confirm that there are no problems in securing airways. All procedures require close communication with the attending physician. If there is leakage of the tube and rupture of the cuff after intubation through the nasal cavity, it is necessary to determine whether there are abnormal C that might cause problems in the tracheal intubation passage through the nasal cavity. In particular, it is necessary to carefully examine patients with fixed micro-implants, as in this case. In other cases, the presence of a nasal spur may damage the cuff, similar to the above case.
Although corrective micro-implants were placed by other dentists during the period between preoperative evaluation and surgery in this case, we regret that we did not confirm the orthodontic micro-implant that was fixed to the hard palate prior to nasotracheal intubation.
Although the timing of preoperative evaluation depends on the patient's schedule, preoperative evaluation including preoperative X-ray is generally performed after micro-implants procedure. In this case, due to the patient's schedule, micro-implant procedure was performed 5 days after preoperative evaluation. Surgery was performed 3 days after the micro-implant procedure. As the time interval between micro-implants procedure and orthognathic surgery was too short, and it X-ray cannot clearly distinguish whether micro-implant was protruded out of the tissue or not, post-implant X-ray was not taken.
Not all patients with orthognathic surgery got micro-implants procedure before surgery. The micro-implant inserted into the palate acts as an anchor for pulling or pushing a tooth. Recently, in patients with narrow maxillary, the uses of mini-screw assisted rapid palatal expansion (MARPE) are increasing. In this patient, MARPE was performed to expand the maxilla thus widen the nasal airway. In general, the micro-implant procedure does not make a problem for intubation because it is located within the tissue in most cases. This is a rare case in which the direction of micro-implant insertion was misaligned, and the tip of micro-implant was protruded out of tissue.
In order to prevent problems such as our case, we suggest to check whether the patients undergoing orthoganthic surgery was performed micro-implants or not, and nasal cavity using nasal endoscopy before surgery if micro-implans was performed. To check the oral cavity before nasal intubation and intubate endotracheal tube to the other side of imcro-implant also would be the help to prevent problems.
In our case, endotracheal tube cuff leakage was not identified during the preoperative evaluation and was resolved through additional alternatives. In the case of intubation through the nasal cavity, it is necessary to proceed with caution because one may encounter various situations.
Notes
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
DATA AVAILABILITY STATEMENT
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
AUTHOR CONTRIBUTIONS
Conceptualization: Su Hyun Seo, Jun Mo Lee, Je Jin Lee, Eun Jin Ahn, Geun Joo Choi, Hyun Kang. Data curation: Su Hyun Seo, Jun Mo Lee, Eun Jin Ahn, Geun Joo Choi. Visualization: Su Hyun Seo, Hyun Kang. Writing - original draft: Su Hyun Seo, Jun Mo Lee, Je Jin Lee, Eun Jin Ahn, Hyun Kang. Writing - review & editing: Geun Joo Choi, Hyun Kang. Supervision: Geun Joo Choi, Hyun Kang. Validation: Hyun Kang.


