Acute traumatic injury and delayed airway obstruction after the use of a GlideScope in a patient with a difficult airway -A case report-
Article information
Abstract
Endotracheal intubation sometimes leads to complications, particularly in patients with anticipated difficult intubation. The GlideScope is preferred because of its high success rate in cases with anticipated difficult intubation. However, complications during the process have been reported. Most minor injuries can be treated after early detection. However, treatment can be difficult if complications occur later. We report a patient who underwent an emergency tracheostomy due to a delayed airway obstruction caused by pharyngeal wall bleeding during intubation with a GlideScope.
INTRODUCTION
Endotracheal intubation is a relatively simple procedure. Most intubations performed by experienced anesthesiologists are uneventful. However, complications may occur during this simple procedure, including upper airway bleeding due to blunt trauma and soft tissue edema. These complications can lead to catastrophic results due to a loss of airway patency [1]. Therefore, careful preparation is needed before performing endotracheal intubation.
The GlideScope (Verathon, Canada) is a device that allows visualization of the glottis without alignment of the oral, pharyngeal, and tracheal axes through a digital camera [2]. It is now used widely when intubating patients with anticipated difficult airways. However, traumatic complications have been reported following use of the GlideScope [3,4]. These reports suggest that physicians must be aware of the possibility of acute and immediate complications following GlideScope use. However, delayed airway complications following GlideScope use have not been widely reported.
Here, we report a case of delayed airway obstruction in a patient who underwent endotracheal intubation with a GlideScope during the induction of general anesthesia. Although there was acute bleeding during intubation, it was self-limiting. The patient did not complain of dyspnea in the recovery room. However, after the patient had been moved to the general ward, abrupt, severe dyspnea occurred and an emergency tracheostomy was performed.
CASE REPORT
A 71-year-old male (168 cm, 71.5 kg, American Society of Anesthesiologists physical status classification II) was admitted for elective vitrectomy under general anesthesia. He was taking medications for hypertension and diabetes. He had undergone the Miles operation 13 years earlier due to rectal cancer without any anesthetic difficulties.
A preoperative electrocardiogram showed left ventricular hypertrophy. No specific lung lesion was found on chest radiography. All standard laboratory test results were normal. An airway assessment before induction showed a normal thyromental distance and full dentition, but poor neck extension (Mallampati grade 2).
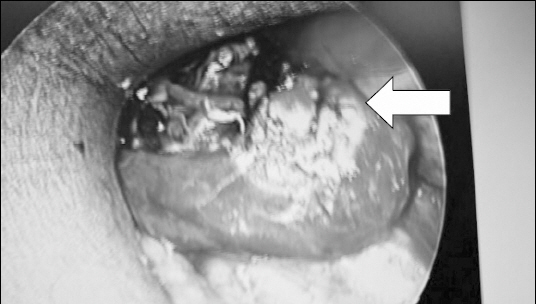
Premedication with 0.2 mg of glycopyrrolate was injected intramuscularly. The initial vital signs in the operating room were as follows: blood pressure (BP) 147/71 mmHg, heart rate (HR) 84 beats/min (bpm), and oxygen saturation 97%. Anesthesia was induced with intravenous propofol (80 mg) and rocuronium (35 mg). An initial laryngoscopic endotracheal intubation was attempted after 3 min of mask ventilation. However, intubation was impossible due to limited neck extension and a poor laryngoscopic view (Cormack-Lehane grade 3). After performing additional mask ventilation without difficulty, a GlideScope was used to perform the intubation. The larynx was well visualized and an 8.0 mm endotracheal tube was inserted into the trachea. However, immediate post-intubation bleeding was discovered and oral suctioning was performed. The bleeding was so slight that it was difficult to quantify in the suction bottle, and suctioning was stopped without any additional treatment. The patient underwent the scheduled operation, which lasted 80 min. The patient was extubated after confirming negative bleeding by direct laryngoscopy. He was given 200 mg of sugammadex and observed in the recovery room for 30 min without any symptoms of bleeding or dyspnea before being transferred to the general ward. The patient felt only mild discomfort on the general ward 1.5 h later (4 h after intubation). However, 30 min after that, he complained of oropharyngeal bleeding and dyspnea. The patient’s vital signs during the initial dyspnea were: BP, 150/80 mmHg; HR, 94 bpm; and respiration rate (RR), 24 breaths/min. Despite oxygen supplementation (2 L/min via nasal prongs), the patient’s symptoms did not improve and his peripheral oxygen saturation decreased to 85%. The rapid response team arrived immediately, but failed to intubate the patient due to pharyngeal wall edema with continuous bleeding. An emergency percutaneous tracheostomy was performed and the patient’s vital signs returned to normal (BP, 142/77 mmHg; HR, 98 bpm; RR, 20 breaths/min; oxygen saturation, 97%). The patient was transferred to the intensive care unit. Neck computed tomography revealed soft tissue swelling of the upper airway and a hematoma with active bleeding in the oropharynx (Fig. 1). An emergency operation was performed under general anesthesia to control the bleeding. During bleeding control, a huge mucosal lesion with continuous bleeding was discovered in the posterior pharyngeal wall (Fig. 2). The patient was transferred to the general ward the following day without any further complications during outpatient follow-up.

Neck computed tomography showing a diffuse soft tissue swelling in the oropharynx and supraglottic area with suspected hemorrhage or hematoma in the airway suggestive of active bleeding.
DISCUSSION
Airway injury during endotracheal intubation is rare, but it can be catastrophic [1]. Risk factors include multiple attempts, inexperienced physicians, inappropriate equipment selection, and abrupt patient actions [5]. Although such complications can be problematic in both the upper and lower airways, we will discuss only upper airway injuries during difficult intubation.
Pharyngeal wall injury can occur with the use of an endotracheal tube, laryngeal mask airway, L-tube, or esophageal stethoscope [6]. When associated with endotracheal intubation, it usually occurs in patients with difficult airways. It can appear as a perforation, laceration, or localized infection [7]. Early symptoms are usually non-specific, including a sore throat, chest pain, and cough. Late symptoms include deep or retropharyngeal abscesses, mediastinitis, and pneumonia [8,9]. The diagnosis of pharyngeal wall injury is often difficult due to the non-specific symptoms [10]. Although some cases can improve without treatment, surgical treatment may be required depending on the severity of the symptoms [7]. Early detection can be achieved immediately during or after surgery because the airway disruption usually occurs acutely [1]. Progression to a catastrophic event can be prevented through early detection. However, delayed symptom onset may interfere with early detection and appropriate treatment. In our case, an upper airway obstruction due to endotracheal intubation was discovered 2 h after the end of surgery in a general ward.
Although early traumatic complications have frequently been reported after the use of a GlideScope [3,4,11], delayed complications have not been reported widely. Since its introduction in 2002, the GlideScope has been used widely due to its high success rates for endotracheal intubation in patients with difficult airways [2]. The enlarged view shown on the GlideScope monitor can be shared with other anesthesiologists, enabling rapid treatment. In addition, its bent tip offers good visualization of structures not observed with a laryngoscope. In a retrospective review of 2,004 cases of GlideScope intubation, Aziz et al. [11] found that the success rate was high in both primary (98% of 1,755) and rescued failed direct laryngoscopy (94% of 239). During intubation with a GlideScope, a rigid styletted endotracheal tube is inserted into the oropharynx blindly in most cases since the anesthesiologist is concentrating on the GlideScope monitor. Traumatic injury to the pharyngeal wall may occur during this process. Therefore, the tip of the endotracheal tube should be kept as close as possible to the blade before it appears on the monitor. In addition, when the oropharyngeal space is narrow due to limited mouth opening or hypertrophic soft tissues, the anesthesiologist tends to lever the blade. Such levering should be avoided because it can increase the “blind spot” area and further decrease the oropharyngeal space [12,13].
In our patient, we did not use a stylet in the first trial, which failed. Intubation succeeded with a styletted endotracheal tube in the second trial. We believe that a styletted tube is less likely to damage the posterior pharyngeal wall because there was no traumatic event involving the soft tissues in either trial. According to an otorhinolaryngologist, the remaining traces of scratches on the posterior pharyngeal wall were likely caused by the GlideScope blade tip. However, the possibility of injury due to the stylet cannot be ruled out completely in this case.
In our case, we confirmed the absence of complications at the end of surgery via direct laryngoscopy. However, we might have missed important traumatic injuries due to the limited view. The use of a GlideScope or bronchoscope before extubation might have prevented such a catastrophic event. In practice, confirmation of a lack of injury by an otorhinolaryngologist might also be required, even following minor bleeding or airway injury.
In conclusion, since most complications occur in patients with difficult airways, it is important to prepare an appropriate intubation strategy for these patients with a proper preoperative evaluation and history. Although traumatic pharyngeal wall bleeding during intubation is rare, it should not be underestimated considering the severity of complications. Anesthesiologists must be aware of the possibility of delayed complications, as seen in our case. When airway damage is suspected during intubation, careful inspection is needed before awakening and extubating the patient.